Non-dipping blood pressure pattern is associated with cardiovascular events in a 21-year follow-up study
IF 2.7
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
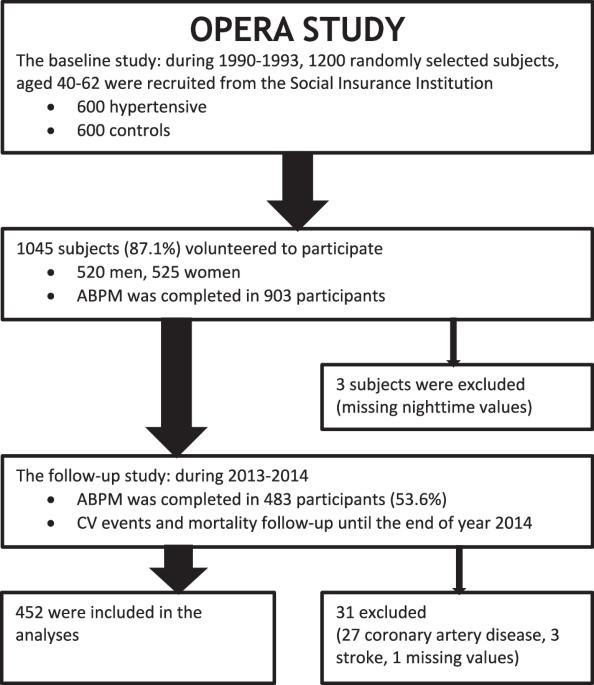
Non-dipping blood pressure (BP) pattern is a predictor for cardiovascular (CV) events and mortality. We evaluated dipping status change and its association with incidence of non-fatal CV events in middle-aged subjects. The OPERA study was carried out during the years 1991–1993, with a follow-up study 21.7 years later. In this study, we included 452 participants with 24-h ambulatory BP measurements (ABPM) available in both surveys. The study population was divided into four groups according to the dipping pattern change: dipping–dipping (n = 152/33.6%), dipping–non-dipping (n = 198/43.8%), non-dipping–dipping (n = 20/4.4%), and non-dipping–non-dipping (n = 82/18.1%). Sixty-five participants experienced a CV event (14.4%) during the 21.7 (SD 0.8) years of follow-up. The incidence of events was highest (28%) in the non-dipping–non-dipping group, and lowest (6.6%) in the dipping–dipping group (p < 0.001). In Cox regression analyses the covariates were age, sex, total cholesterol, hypertension and use of antihypertensive medication, systolic office BP and ambulatory mean or nighttime systolic BP, as well as the change in the variables during the follow-up period. After adjustments, the association of the non-dipping–non-dipping pattern with CV events compared with the dipping–dipping pattern remained significant (HR 4.01; 95% CI 1.89–8.67, p < 0.001). In summary, non-dipping–non-dipping pattern was associated with non-fatal CV events in the long term, and the effect was independent of the conventional risk factors including office and ambulatory BP levels.
一项为期 21 年的随访研究显示,非骤降血压模式与心血管事件有关
非滂沱血压(BP)模式是心血管(CV)事件和死亡率的预测因素。我们评估了中年受试者的降压状态变化及其与非致死性心血管事件发生率的关系。OPERA 研究于 1991-1993 年间进行,21.7 年后进行了随访研究。在这项研究中,我们纳入了 452 名在两次调查中都进行了 24 小时动态血压测量(ABPM)的参与者。根据浸润模式的变化,研究人群被分为四组:浸润-浸润(n = 152/33.6%)、浸润-非浸润(n = 198/43.8%)、非浸润-非浸润(n = 20/4.4%)和非浸润-非浸润(n = 82/18.1%)。在 21.7 (SD 0.8) 年的随访期间,65 名参与者发生了冠心病事件(14.4%)。非浸渍-非浸渍组的事件发生率最高(28%),浸渍-浸渍组的事件发生率最低(6.6%)(p < 0.001)。在 Cox 回归分析中,协变量包括年龄、性别、总胆固醇、高血压和使用降压药、办公室收缩压和流动平均或夜间收缩压,以及随访期间变量的变化。经调整后,与浸渍-浸渍模式相比,非浸渍-非浸渍模式与冠心病事件的关系仍然显著(HR 4.01; 95% CI 1.89-8.67, p <0.001)。总之,长期来看,非浸渍-非浸渍模式与非致死性冠心病事件相关,而且这种影响与传统的风险因素(包括诊室血压和非卧床血压水平)无关。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


