Prognostic value of cardiovascular magnetic resonance in immune checkpoint inhibitor-associated myocarditis: A systematic review and meta-analysis
Abstract
Background
Immune checkpoint inhibitors (ICI) are increasingly used in the first-line treatment of malignant tumors. There is increasing recognition of their cardiotoxicity and, in particular, their potential to lead to myocarditis. Cardiovascular magnetic resonance (CMR) can quantify pathological changes, such as myocardial edema and fibrosis. The purpose of this systematic review and meta-analysis was to examine the evidence for the roles of CMR in predicting prognosis in ICI-associated myocarditis.
Methods
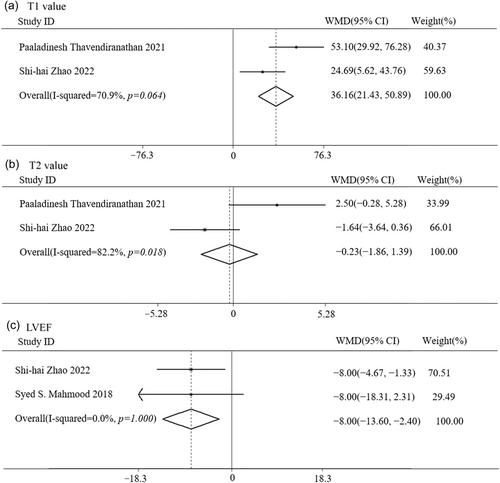
PubMed, Cochrane Library, and Web of Science databases were searched until October 2023 for published works investigating the relationship between CMR parameters and adverse events in patients with ICI-associated myocarditis. The analysis included studies reporting the incidence of late gadolinium enhancement (LGE), T1 values, T2 values, and CMR-derived left ventricular ejection fraction (LVEF). Odds ratios (OR) and weighted mean differences (WMD) were combined for binary and continuous data, respectively. Newcastle-Ottawa Scale was used to assess the methodological quality of the included studies.
Results
Five cohort studies were included (average age 65–68 years; 25.4% female). Of these, four studies were included in the meta-analysis of LGE-related findings. Patients with major adverse cardiovascular events (MACE) had a higher incidence of LGE compared with patients without MACE (OR = 4.18, 95% CI: 1.72–10.19, p = 0.002). A meta-analysis, incorporating data from two studies, showed that patients who developed MACE exhibited significantly higher T1 value (WMD = 36.16 ms, 95% CI: 21.43–50.89, p < 0.001) and lower LVEF (WMD = − 8.00%, 95% CI: −13.60 to −2.40, p = 0.005). Notably, T2 value (WMD = −0.23 ms, 95% CI: −1.86 to −1.39, p = 0.779) was not associated with MACE in patients with ICI-related myocarditis.
Conclusions
LGE, T1 value, and LVEF measured by CMR imaging have potential prognostic value for long-term adverse events in patients with ICI-related myocarditis.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


