Establishment of a humanized mouse model using steady-state peripheral blood-derived hematopoietic stem and progenitor cells facilitates screening of cancer-targeted T-cell repertoires
Abstract
Background
Cancer-targeted T-cell receptor T (TCR-T) cells hold promise in treating cancers such as hematological malignancies and breast cancers. However, approaches to obtain cancer-reactive TCR-T cells have been unsuccessful.
Methods
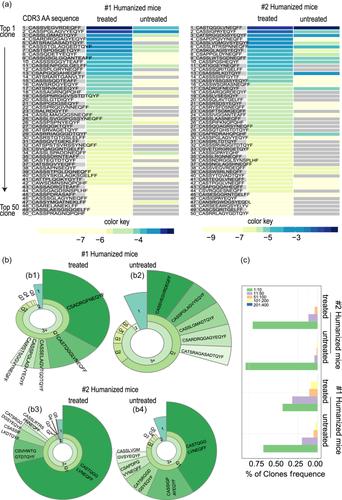
Here, we developed a novel strategy to screen for cancer-targeted TCR-T cells using a special humanized mouse model with person-specific immune fingerprints. Rare steady-state circulating hematopoietic stem and progenitor cells were expanded via three-dimensional culture of steady-state peripheral blood mononuclear cells, and then the expanded cells were applied to establish humanized mice. The human immune system was evaluated according to the kinetics of dendritic cells, monocytes, T-cell subsets, and cytokines. To fully stimulate the immune response and to obtain B-cell precursor NAML-6- and triple-negative breast cancer MDA-MB-231-targeted TCR-T cells, we used the inactivated cells above to treat humanized mice twice a day every 7 days. Then, human T cells were processed for TCR β-chain (TRB) sequencing analysis. After the repertoires had been constructed, features such as the fraction, diversity, and immune signature were investigated.
Results
The results demonstrated an increase in diversity and clonality of T cells after treatment. The preferential usage and features of TRBV, TRBJ, and the V–J combination were also changed. The stress also induced highly clonal expansion. Tumor burden and survival analysis demonstrated that stress induction could significantly inhibit the growth of subsequently transfused live tumor cells and prolong the survival of the humanized mice.
Conclusions
We constructed a personalized humanized mouse model to screen cancer-targeted TCR-T pools. Our platform provides an effective source of cancer-targeted TCR-T cells and allows for the design of patient-specific engineered T cells. It therefore has the potential to greatly benefit cancer treatment.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


