Exploring the utility of bedside tests for predicting cardiorespiratory fitness in older adults
Abstract
Objectives
Cardiorespiratory fitness (CRF) declines with advancing and has also, independent of age, been shown to be predictive of all-cause mortality, morbidity, and poor clinical outcomes. In relation to the older patient, there is a particular wealth of evidence highlighting the relationship between low CRF and poor surgical outcomes. Cardiopulmonary exercise testing (CPET) is accepted as the gold-standard measure of CRF. However, this form of assessment has significant personnel and equipment demands and is not feasible for those with certain age-associated physical limitations, including joint and cardiovascular comorbidities. As such, alternative ways to assess the CRF of older patients are very much needed.
Methods
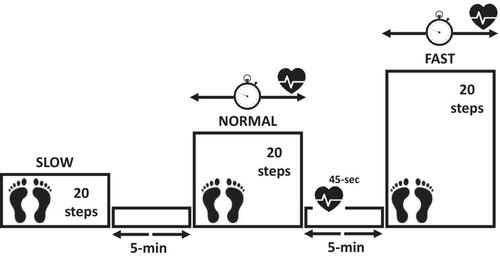
Sixty-four participants (45% female) with a median age of 74 (65–90) years were recruited to this study via community-based advertisements. All participants completed three tests of physical function: (1) a step-box test; (2) handgrip strength dynamometry; and (3) a CPET on a cycle ergometer; and also had their muscle architecture (vastus lateralis) assessed by B-mode ultrasonography to provide measures of muscle thickness, pennation angle, and fascicle length. Multivariate linear regression was then used to ascertain bedside predictors of CPET parameters from the alternative measures of physical function and demographic (age, gender, body mass index (BMI)) data.
Results
There was no significant association between ultrasound-assessed parameters of muscle architecture and measures of CRF. VO2peak was predicted to some extent from fast step time during the step-box test, gender, and BMI, leading to a model that achieved an R2 of 0.40 (p < 0.001). Further, in aiming to develop a model with minimal assessment demands (i.e., using handgrip dynamometry rather than the step-box test), replacing fast step time with non-dominant HGS led to a model which achieved an R2 of 0.36 (p < 0.001). Non-dominant handgrip strength combined with the step-box test parameter of fast step time and BMI delivered the most predictive model for VO2peak with an R2 of 0.45 (p < 0.001).
Conclusions
Our findings show that simple-to-ascertain patient characteristics and bedside assessments of physical function are able to predict CPET-derived CRF. Combined with gender and BMI, both handgrip strength and fast step time during a step-box test were predictive for VO2peak. Future work should apply this model to a clinical population to determine its utility in this setting and to explore if simple bedside tests are predictive of important clinical outcomes in older adults (i.e., post-surgical complications).

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


