Relationship between 24 h blood pressure variability and mortality in acute myocardial infarction patients
Abstract
Background
In recent years, the mortality of patients with AMI has not declined significantly. The relationship between blood pressure variability (BPV) and acute myocardial infarction (AMI) is unclear. We explored the relationship between 24-h BPV and mortality in patients with AMI.
Hypothesis
The mortality of patients with AMI is related to BPV. We hope to provide therapeutic ideas for reducing the risk of death in patients with AMI.
Methods
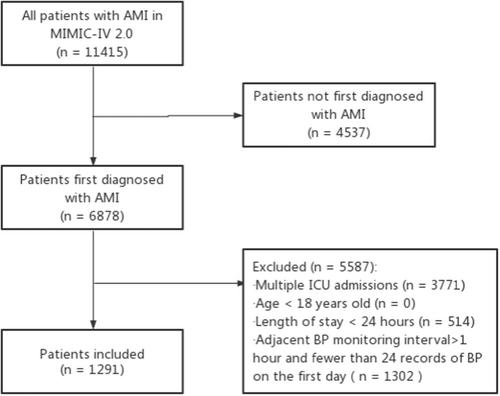
This is a retrospective cohort study. We extracted and analyzed data from the MIMIC-IV 2.0, which was established in 1999 under the auspices of the National Institutes of Health (America). The average real variability (ARV) was calculated for the first 24-h blood pressure measurement after patients with AMI were admitted to the intensive care unit (ICU). Patients were divided into four groups according to ARV quartiles. The outcomes were 30-day, 1-year, and 3-year all-cause mortalities. Data were analyzed using Cox regression, Kaplan–Meier curves, and restricted cubic spline (RCS) curves.
Results
We enrolled 1291 patients with AMI, including 475 female. The patients were divided into four groups according to the qualities of diastolic blood pressure (DBP)-ARV. There were significant differences in the 30-day, 1-year and 3-year mortality among the four groups (p = .02, p < .001, p < .001, respectively). After adjustment for confounding factors, systolic blood pressure (SBP)-ARV could not predict AMI patient mortality (p > .05), while the highest DBP-ARV was associated strongly with increased 30-day mortality (HR: 2.291, 95% CI 1.260-4.168), 1-year mortality (HR: 1.933, 95% CI 1.316-2.840) and 3-year mortality (HR: 1.743, 95% CI 1.235-2.461). Kaplan–Meier curves demonstrated that, regardless of SBP or DBP, the long-term survival probabilities of patients in the highest ARV group were significantly lower than that of those in other groups. RCS curves showed that the death risk of patients with AMI first decreased and then increased with the increase in ARV when DBP-ARV < 8.04. The 30-day death risk first increased and then decreased, and the 1-year and 3-year death risks increased and then stabilized with ARV increase when DBP-ARV > 8.04.
Conclusion
This study showed that patients with AMI may have an increased risk of short- and long-term death if their DBP-ARV is higher or lower during the first 24-h in ICU.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


