TRBC1-targeting antibody–drug conjugates for the treatment of T cell cancers
IF 50.5
1区 综合性期刊
Q1 MULTIDISCIPLINARY SCIENCES
引用次数: 0
Abstract
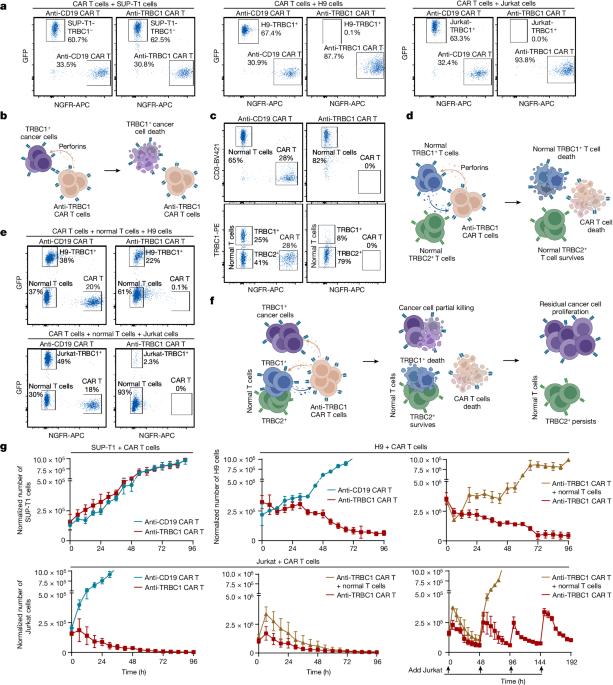
Antibody and chimeric antigen receptor (CAR) T cell-mediated targeted therapies have improved survival in patients with solid and haematologic malignancies1–9. Adults with T cell leukaemias and lymphomas, collectively called T cell cancers, have short survival10,11 and lack such targeted therapies. Thus, T cell cancers particularly warrant the development of CAR T cells and antibodies to improve patient outcomes. Preclinical studies showed that targeting T cell receptor β-chain constant region 1 (TRBC1) can kill cancerous T cells while preserving sufficient healthy T cells to maintain immunity12, making TRBC1 an attractive target to treat T cell cancers. However, the first-in-human clinical trial of anti-TRBC1 CAR T cells reported a low response rate and unexplained loss of anti-TRBC1 CAR T cells13,14. Here we demonstrate that CAR T cells are lost due to killing by the patient’s normal T cells, reducing their efficacy. To circumvent this issue, we developed an antibody–drug conjugate that could kill TRBC1+ cancer cells in vitro and cure human T cell cancers in mouse models. The anti-TRBC1 antibody–drug conjugate may provide an optimal format for TRBC1 targeting and produce superior responses in patients with T cell cancers. Anti-TRBC1 antibody–drug conjugates may offer a more potent T cell cancer therapy by bypassing the fratricide that may be limiting the efficacy of anti-TRBC1 CAR T cells in the clinical trial for patients with T cell cancers.

用于治疗 T 细胞癌症的 TRBC1 靶向抗体-药物共轭物。
抗体和嵌合抗原受体(CAR)T 细胞介导的靶向疗法提高了实体瘤和血液恶性肿瘤患者的生存率1-9。成人 T 细胞白血病和淋巴瘤(统称为 T 细胞癌)患者的生存期较短10,11 ,且缺乏此类靶向疗法。因此,T 细胞癌症尤其需要开发 CAR T 细胞和抗体,以改善患者的预后。临床前研究表明,靶向 T 细胞受体 β 链恒定区 1(TRBC1)可以杀死癌变 T 细胞,同时保留足够的健康 T 细胞以维持免疫力12,这使得 TRBC1 成为治疗 T 细胞癌的一个有吸引力的靶点。然而,抗TRBC1 CAR T细胞的首次人体临床试验报告显示,抗TRBC1 CAR T细胞的应答率很低,而且抗TRBC1 CAR T细胞的丢失原因不明13,14。我们在这里证明,CAR T 细胞会因患者正常 T 细胞的杀伤而丢失,从而降低其疗效。为了避免这一问题,我们开发了一种抗体-药物共轭物,它可以在体外杀死 TRBC1+ 癌细胞,并在小鼠模型中治愈人类 T 细胞癌症。抗 TRBC1 抗体-药物共轭物可为 TRBC1 靶向提供最佳形式,并对 T 细胞癌症患者产生卓越的反应。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Nature
综合性期刊-综合性期刊
CiteScore
90.00
自引率
1.20%
发文量
3652
审稿时长
3 months
期刊介绍:
Nature is a prestigious international journal that publishes peer-reviewed research in various scientific and technological fields. The selection of articles is based on criteria such as originality, importance, interdisciplinary relevance, timeliness, accessibility, elegance, and surprising conclusions. In addition to showcasing significant scientific advances, Nature delivers rapid, authoritative, insightful news, and interpretation of current and upcoming trends impacting science, scientists, and the broader public. The journal serves a dual purpose: firstly, to promptly share noteworthy scientific advances and foster discussions among scientists, and secondly, to ensure the swift dissemination of scientific results globally, emphasizing their significance for knowledge, culture, and daily life.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


