Implementation frameworks guiding digital self-management intervention in chronic pain: A scoping review
Abstract
Background and Objective
The development, evaluation and implementation of digital self-management interventions for chronic pain have increased exponentially. While intervention outcomes appear promising to improve well-being and functioning in target populations, it is unclear how the development and evaluation processes were structured and how implementation was planned and executed. The aim of this systematic review is to provide a comprehensive overview of implementation frameworks used to guide and evaluate scientific innovation in chronic pain.
Databases and Data Treatment
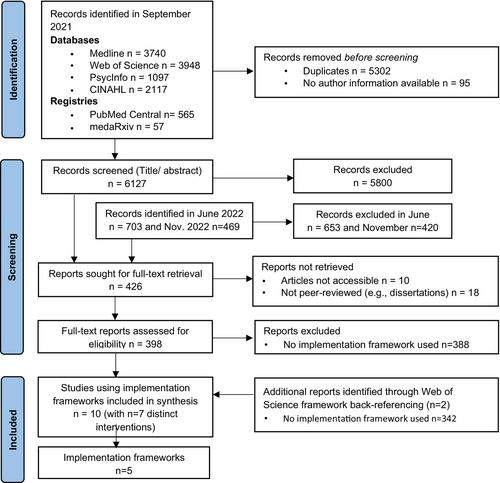
Four bibliography databases (Medline, Web of Science, PsycInfo, CINAHL) and two registries (PubMed Central, MedaRxiv) were systematically searched. Hits (n = 6830) and full texts (n = 351) were screened and read by two independent reviewers. Peer-reviewed articles that met the inclusion criteria were included in the narrative synthesis.
Results
In total, 10 studies were identified that report on seven distinct interventions. Five implementation frameworks were utilized across these studies: Behavioural Interventions using Technology (BIT); Consolidated Framework for Implementation Research (CFIR); mHealth Agile and User-Centered Research and Development Lifecycle; Medical Research Council (MRC); Reach, Effectiveness, Adoption Implementation, and Maintenance (RE-AIM). Frameworks were operationalized using qualitative and quantitative methods, evaluating the innovation on various levels (e.g., individual vs. organizational) and applying a variety of study designs (e.g., single-arm or large trials).
Conclusions
By utilizing implementation frameworks, access to evidence-based chronic pain care may be increased. Although the evidence on the utility of implementation frameworks to guide and evaluate digital self-management interventions is still limited, the body of literature is increasing. Future studies are urged to operationalize, communicate and discuss the innovation process, to promote transparency and replicability.
Significance
The use of implementation frameworks to guide and evaluate digital self-management interventions for chronic pain is a recent development in the field. Several promising examples exist and are presented in this review. Currently, the evidence is still limited, and prospective studies need to transparently operationalize, communicate and discuss their efforts. By utilizing an implementation framework, promising interventions can be made available to end-users, closing the research-to-clinical practice gap and increasing access to evidence-based care to people with chronic pain.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


