The clinical benefits of sodium–glucose cotransporter type 2 inhibitors in people with gout
IF 29.4
1区 医学
Q1 RHEUMATOLOGY
引用次数: 0
Abstract
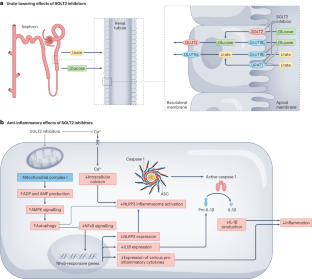
Gout is the most common form of inflammatory arthritis worldwide and is characterized by painful recurrent flares of inflammatory arthritis that are associated with a transiently increased risk of adverse cardiovascular events. Furthermore, gout is associated with multiple cardiometabolic–renal comorbidities such as type 2 diabetes, chronic kidney disease and cardiovascular disease. These comorbidities, potentially combined with gout flare-related inflammation, contribute to persistent premature mortality in gout, independently of serum urate concentrations and traditional cardiovascular risk factors. Although better implementation of standard gout care could improve gout outcomes, deliberate efforts to address the cardiovascular risk in patients with gout are likely to be required to reduce mortality. Sodium–glucose cotransporter type 2 (SGLT2) inhibitors are approved for multiple indications owing to their ability to lower the risk of all-cause and cardiovascular death, hospitalizations for heart failure and chronic kidney disease progression, making them an attractive treatment option for gout. These medications have also been shown to lower serum urate concentrations, the causal culprit in gout risk, and are associated with a reduced risk of incident and recurrent gout, potentially owing to their purported anti-inflammatory effects. Thus, SGLT2 inhibition could simultaneously address both the symptoms of gout and its comorbidities. Gout is associated with various cardiometabolic–renal comorbidities that increase the risk of mortality. Sodium–glucose cotransporter type 2 (SGLT2) inhibitors show promise in both addressing the symptoms of gout and managing relevant comorbidities to help prevent premature mortality.
钠-葡萄糖共转运体 2 型抑制剂对痛风患者的临床益处。
痛风是全球最常见的炎症性关节炎,其特点是炎症性关节炎反复发作,疼痛难忍,与不良心血管事件风险的短暂增加有关。此外,痛风还与多种心脏代谢-肾脏合并症有关,如 2 型糖尿病、慢性肾脏病和心血管疾病。这些合并症可能与痛风发作相关的炎症相结合,导致痛风患者持续过早死亡,而不受血清尿酸盐浓度和传统心血管风险因素的影响。虽然更好地实施标准痛风治疗可以改善痛风的治疗效果,但要降低死亡率,可能还需要刻意降低痛风患者的心血管风险。钠-葡萄糖共转运体2型(SGLT2)抑制剂由于能够降低全因和心血管疾病死亡、心力衰竭住院和慢性肾病恶化的风险而被批准用于多种适应症,这使其成为治疗痛风的一种有吸引力的选择。这些药物还被证明能降低血清尿酸盐浓度(痛风风险的罪魁祸首),并能降低痛风发生和复发的风险,这可能是由于它们所谓的抗炎作用。因此,SGLT2 抑制剂可以同时治疗痛风症状及其合并症。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Nature Reviews Rheumatology
医学-风湿病学
CiteScore
29.90
自引率
0.90%
发文量
137
审稿时长
6-12 weeks
期刊介绍:
Nature Reviews Rheumatology is part of the Nature Reviews portfolio of journals. The journal scope covers the entire spectrum of rheumatology research. We ensure that our articles are accessible to the widest possible audience.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


