Clinical characteristics of new-onset diabetes after liver transplantation and outcomes
Abstract
Background
We aimed to identify the characteristics of new-onset diabetes after liver transplantation (LT) (NODAT) and investigate its impacts on post-transplant outcomes.
Methods
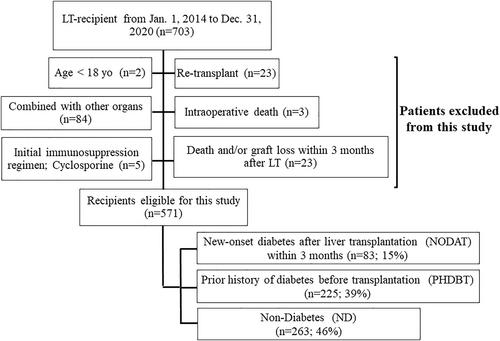
Adult LT patients between 2014 and 2020 who used tacrolimus as initial immunosuppression and survived 3 months at least were evaluated. Patients who developed NODAT within 3 months after LT were classified as NODAT group. Also, patients were further classified as history of diabetes before LT (PHDBT) and non-diabetes (ND) groups. Patient characteristics, post-LT outcomes, and cardiovascular and/or pulmonary complications were compared.
Results
A total of 83, 225, and 263 patients were classified into NODAT, PHDBT, and ND groups. The proportion of cholestatic liver disease and rejection within 90 days were higher in NODAT group. Mean serum tacrolimus concentration trough level in the first week after LT was 7.12, 6.12, and 6.12 ng/mL (p < 0.001). Duration of corticosteroids was significantly longer in NODAT compared to PHDBD or ND (416, 289, and 228 days, p < 0.001). Three-year graft and patient survival were significantly worse in NODAT than ND (80.5% vs. 95.0%, p < 0.001: 82.0% vs. 95.4%, p < 0.001) but similar to PHDBT. Adjusted risks of 3-year graft loss and patient death using Cox regression analysis were significantly higher in NODAT compared to ND (adjusted hazard ratio [aHR] 3.41, p = 0.004; aHR 3.61, p = 0.004). Incidence rates of cardiovascular or pulmonary complications after LT in NODAT were significantly higher than ND but similar to PHDBT.
Conclusion
Higher initial tacrolimus concentration and early rejection might be risk factors for NODAT. NODAT was associated with worse post-transplant outcomes.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


