Individual versus integration of multiple components of central blood pressure and aortic stiffness in predicting cardiovascular mortality in end-stage renal diseases
IF 3.4
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
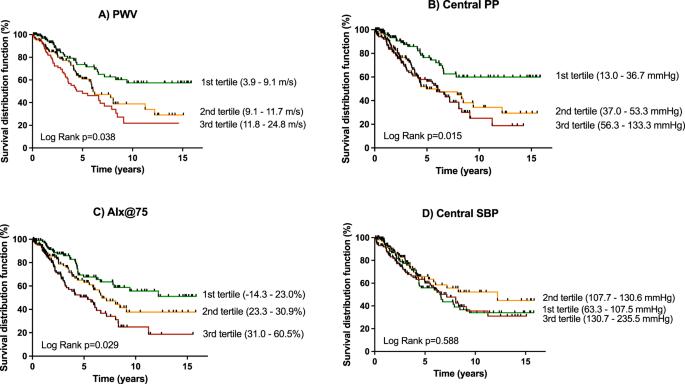
Aortic stiffness, measured by carotid-femoral pulse wave velocity (PWV), is a predictor of cardiovascular (CV) mortality in patients with end-stage renal disease (ESRD). Aortic stiffness increases aortic systolic and pulse pressures (cSBP, cPP) and augmentation index adjusted for a heart rate of 75 beats per minute (AIx@75). In this study, we examined if the integration of multiple components of central blood pressure and aortic stiffness (ICPS) into risk score categories could improve CV mortality prediction in ESRD. In a prospective cohort of 311 patients with ESRD on dialysis who underwent vascular assessment at baseline, 118 CV deaths occurred after a median follow-up of 3.1 years. The relationship between hemodynamic parameters and CV mortality was analyzed through Kaplan–Meier and Cox survival analysis. ICPS risk score from 0 to 5 points were calculated from points given to tertiles, and were regrouped into three risk categories (Average, High, Very-High). A strong association was found between the ICPS risk categories and CV mortality (High risk HR = 2.20, 95% CI: 1.05–4.62, P = 0.036); Very-High risk (HR = 4.44, 95% CI: 2.21–8.92, P < 0.001) as compared to the Average risk group. The Very-High risk category remained associated with CV mortality (HR = 3.55, 95% CI: 1.37–9.21, P = 0.009) after adjustment for traditional CV risk factors as compared to the Average risk group. While higher C-statistics value of ICPS categories (C: 0.627, 95% CI: 0.578–0.676, P = 0.001) was not statistically superior to PWV, cPP or AIx@75, the use of ICPS categories resulted in a continuous net reclassification index of 0.56 (95% CI: 0.07–0.99). In conclusion, integration of multiple components of central blood pressure and aortic stiffness may potentially be useful for better prediction of CV mortality in this cohort.
在预测终末期肾病患者心血管死亡率时,中心血压和主动脉僵硬度多个组成部分的单独预测与综合预测的比较
通过颈动脉-股动脉脉搏波速度(PWV)测量的主动脉僵化可预测终末期肾病(ESRD)患者的心血管(CV)死亡率。主动脉僵化会增加主动脉收缩压和脉搏压(cSBP、cPP)以及按每分钟 75 次心率调整的增强指数(AIx@75)。在这项研究中,我们探讨了将中心血压和主动脉僵硬度(ICPS)的多个组成部分整合到风险评分类别中是否能改善 ESRD 患者的心血管死亡率预测。在一个前瞻性队列中,有 311 名 ESRD 透析患者在基线时接受了血管评估,在中位随访 3.1 年后,有 118 例冠心病死亡。通过卡普兰-梅耶尔和考克斯生存分析法分析了血液动力学参数与冠心病死亡率之间的关系。ICPS 风险评分从 0 分到 5 分,按三等分计算,并重新分为三个风险类别(平均、高、极高)。与平均风险组相比,ICPS 风险类别与冠心病死亡率之间存在很强的关联性(高风险 HR = 2.20,95% CI:1.05-4.62,P = 0.036);极高风险(HR = 4.44,95% CI:2.21-8.92,P <0.001)。与普通风险组相比,在对传统的心血管风险因素进行调整后,极高风险组仍与心血管死亡率相关(HR = 3.55,95% CI:1.37-9.21,P = 0.009)。虽然 ICPS 类别的 C 统计量值更高(C:0.627,95% CI:0.578-0.676,P = 0.001),但在统计学上并不优于脉搏波速度、cPP 或 AIx@75,使用 ICPS 类别可获得 0.56(95% CI:0.07-0.99)的连续净再分类指数。总之,整合中心血压和主动脉僵化的多个组成部分可能有助于更好地预测该队列中的心血管疾病死亡率。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


