Efficacy and safety of mineralocorticoid receptor antagonists for the treatment of low-renin hypertension: a systematic review and meta-analysis
IF 3.4
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
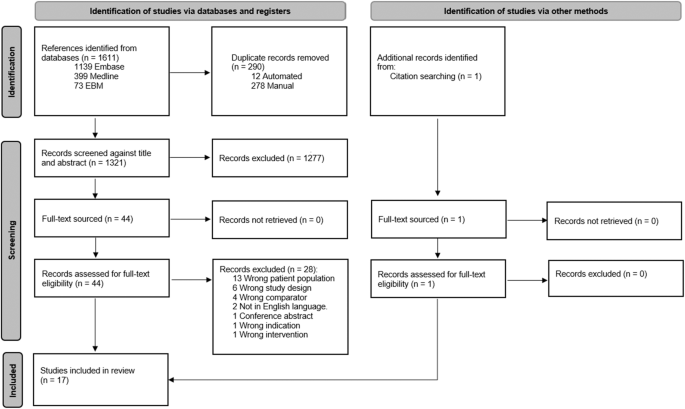
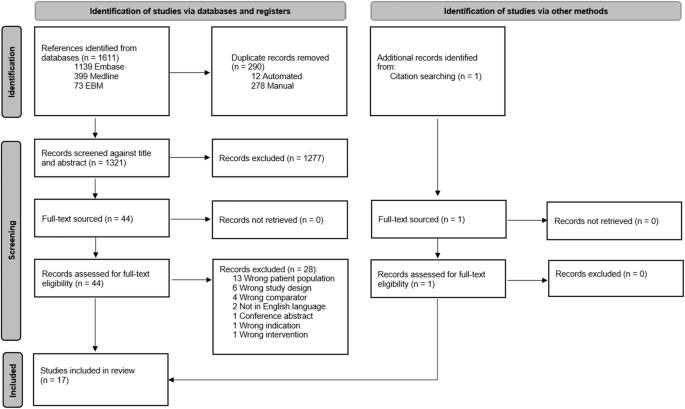
Hypertension is the leading risk factor for premature death. The optimal treatment of low-renin hypertension (LRH), present in 30% of hypertensive individuals, is not known. LRH likely reflects a state of excess salt, expanded volume and/or mineralocorticoid receptor (MR) activation. Therefore, targeted treatment with MR antagonists (MRA) may be beneficial. The objective of this systematic review was to assess the efficacy of MRA therapy in LRH. MEDLINE, Embase and Cochrane databases were searched for randomised controlled trials of adults with LRH that compared the efficacy of MRA to placebo or other antihypertensive treatments. Risk of bias was assessed using the Cochrane risk of bias tool. A meta-analysis was performed using a random-effects model to estimate the difference in blood pressure and the certainty of evidence was assessed using the GRADE approach. The protocol is registered on PROSPERO (CRD42022318763). From the 1612 records identified, 17 studies met the inclusion criteria with a total sample size of 1043 participants. Seven studies (n = 345) were assessed as having a high risk of bias. Meta-analysis indicated that MRA reduced systolic blood pressure by −6.8 mmHg (95% confidence interval −9.6 to −4.1) and −4.8 mmHg (95% confidence interval −11.9 to 2.4) compared to angiotensin-converting enzyme inhibitors/angiotensin receptor blockers (ACEi/ARB) and diuretics. The certainty of the evidence was assessed as moderate and very low, respectively. The findings of this systematic review suggest that MRA is effective in lowering blood pressure in LRH and may be better than ACEi/ARB. Translation to clinical practice is limited by the uncertainty of evidence.
矿物皮质激素受体拮抗剂治疗低肾素高血压的有效性和安全性:系统回顾和荟萃分析。
高血压是导致过早死亡的首要风险因素。30%的高血压患者存在低肾素高血压(LRH),其最佳治疗方法尚不清楚。低肾素高血压可能反映了盐分过多、血容量增加和/或矿质皮质激素受体(MR)激活的状态。因此,使用 MR 拮抗剂 (MRA) 进行有针对性的治疗可能是有益的。本系统综述旨在评估 MRA 治疗 LRH 的疗效。在 MEDLINE、Embase 和 Cochrane 数据库中检索了针对成人 LRH 患者的随机对照试验,这些试验比较了 MRA 与安慰剂或其他降压治疗的疗效。使用 Cochrane 偏倚风险工具对偏倚风险进行了评估。使用随机效应模型进行荟萃分析,以估算血压差异,并使用 GRADE 方法评估证据的确定性。该研究方案已在 PROSPERO(CRD42022318763)上注册。在已确定的 1612 条记录中,有 17 项研究符合纳入标准,总样本量为 1043 人。七项研究(n = 345)被评估为偏倚风险较高。Meta 分析表明,与血管紧张素转换酶抑制剂/血管紧张素受体阻滞剂(ACEi/ARB)和利尿剂相比,MRA 可使收缩压分别降低 -6.8 mmHg(95% 置信区间为 -9.6 至 -4.1)和 -4.8 mmHg(95% 置信区间为 -11.9 至 2.4)。证据的确定性分别被评定为中度和极低。本系统综述的结果表明,MRA 可有效降低 LRH 患者的血压,其效果可能优于 ACEi/ARB。由于证据的不确定性,其在临床实践中的应用受到了限制。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


