The association of ideal cardiovascular health metrics and incident hypertension among an urban population of Iran: a decade follow-up in Tehran Lipid and Glucose Study
IF 2.7
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
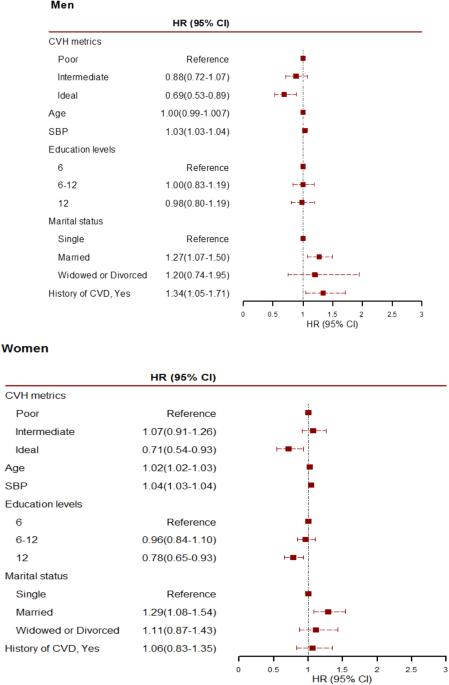
We aimed to determine the association between ideal cardiovascular health metrics (ICVHM) and the incidence of hypertension among Iranian adults. The study population included 5409 Iranian adults aged ≥20 years (2088 men) without hypertension (applying the 2017 American College of Cardiology (ACC)/American Heart Association (AHA) guideline) at baseline. The ICVHM was defined according to the AHA’s 2020 impact goals, excluding total cholesterol was replaced by non-HDL cholesterol (non-HDL-C). Multivariable Cox proportional hazards regression analysis was done to estimate the hazard ratios (HRs) for ICVHM both as continuous and categorical variables. During a median 8.5-year follow-up, 2972 new cases of hypertension were identified (men: 1,287). Non-HDL-C < 130 mg/dL in men [HR (95% CI): 0.75(0.65–0.86)] and fasting plasma glucose(FPG) < 100 mg/dL in women[HR (95% CI): 0.79(0.64–0.97)], and among both genders, being normal/overweigth status (compared to obese) and blood pressure <120/80 mmHg were associated with a lower risk for hypertension. Additionally, in both gender, a 1-point increase in the number of global ICVHM decreased the risk of hypertension by more than 10%, and having ≥5 vs. <2 ICVHM, were associated with a lower risk of hypertension by 30% (all p values < 0.05). Applying the JNC 7 guideline, the association between ICVHM, with incident hypertension, were generally similar. Having a higher number of ICVHM was associated with a lower risk of incident hypertension, using both 2017 ACC/AHA and JNC 7 guidelines, mostly attributable to keeping the ideal status of body mass index, non-HDL-C, and FPG.

伊朗城市人口中理想的心血管健康指标与高血压发病率之间的关系:德黑兰血脂和血糖研究的十年跟踪调查
我们旨在确定伊朗成年人理想心血管健康指标(ICVHM)与高血压发病率之间的关联。研究人群包括 5409 名年龄≥20 岁的伊朗成年人(2088 名男性),他们基线时没有高血压(采用 2017 年美国心脏病学会 (ACC)/ 美国心脏协会 (AHA) 指南)。ICVHM是根据AHA的2020年影响目标定义的,不包括总胆固醇被非高密度脂蛋白胆固醇(non-HDL-C)取代。多变量考克斯比例危险回归分析估算了连续变量和分类变量 ICVHM 的危险比 (HRs)。在中位 8.5 年的随访期间,共发现 2972 例新的高血压病例(男性:1287 例)。男性非高密度脂蛋白胆固醇为 130 毫克/分升[HR (95% CI):0.75(0.65-0.86)],女性空腹血浆葡萄糖为 100 毫克/分升[HR (95% CI):0.79(0.64-0.97)],在男女两性中,体重正常/超重(与肥胖相比)和血压为 120/80 毫米汞柱与较低的高血压风险有关。此外,在男女两性中,全球 ICVHM 的数量每增加 1 个点,患高血压的风险就会降低 10%以上;ICVHM ≥5 与 <2 相比,患高血压的风险降低 30%(所有 p 值均为 <0.05)。根据 JNC 7 指南,ICVHM 与高血压发病率之间的关系大致相似。采用2017 ACC/AHA和JNC 7指南,拥有较多的ICVHM与较低的高血压发病风险有关,这主要归因于保持理想的体重指数、非高密度脂蛋白胆固醇和脂蛋白胆固醇。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


