Blood regulator of G protein signalling 1 as a potential prognostic biomarker in surgical nonsmall cell lung cancer patients: Correlation with clinical features and survival
Abstract
Introduction
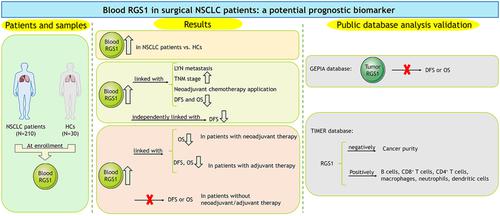
Regulator of G protein signalling 1 (RGS1) closely regulates malignant phenotypes and tumour immunity in several cancers, while its clinical value in nonsmall cell lung cancer (NSCLC) is by far rarely reported. Consequently, this study aimed to explore the linkage of blood RGS1 with clinical features and prognosis in surgical NSCLC patients.
Methods
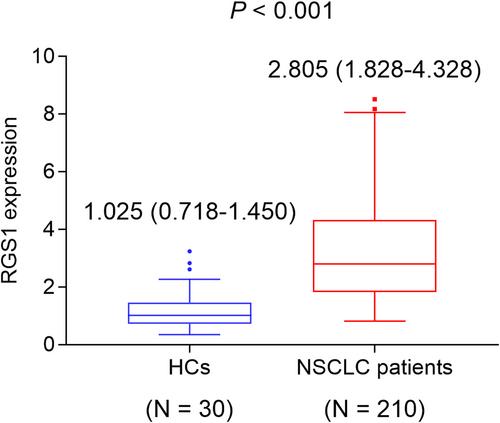
Two-hundred and ten surgical NSCLC patients were consecutively enrolled in this study, whose RGS1 in peripheral blood mononuclear cells was determined before treatment via reverse transcriptional-quantitative polymerase chain reaction. Additionally, the blood RGS1 was also collected from 30 healthy controls (HCs).
Results
Blood RGS1 was increased in NSCLC patients compared with HCs (P < 0.001). Elevated blood RGS1 was related to lymph node (LYN) metastasis (P = 0.001), higher tumour-nodes-metastasis (TNM) stage (P = 0.004), neoadjuvant chemotherapy administration (P = 0.044), shortened accumulative disease-free survival (DFS) (P = 0.008) and overall survival (OS) (P = 0.013) in NSCLC patients. A multivariate Cox's regression analysis showed that blood RGS1 high expression could independently reflect shortened DFS (hazard ratio = 1.499, P = 0.023), whereas it could not independently predict OS (P > 0.050). Furthermore, blood RGS1 high expression was associated with shortened OS (P = 0.020) in patients with neoadjuvant therapy and with worse DFS (P = 0.028) and OS (P = 0.026) in patients with adjuvant therapy, while blood RGS1 was not linked with DFS or OS in patients without neoadjuvant or adjuvant therapy (all P > 0.050).
Conclusion
Elevated blood RGS1 correlates with LYN metastasis, neoadjuvant chemotherapy administration, worse DFS and OS, which might serve as a useful prognostic biomarker for surgical NSCLC patients.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


