Testing feasibility of relevant outcome measures in an inpatient setting to demonstrate the value of occupational therapy
Abstract
Introduction
Measures of participation restrictions in daily life occupations are not typically used and may aid discharge planning and demonstrate the impact of occupational therapy services in inpatient settings. The overall aim of this mixed-methods study was to test the feasibility of relevant outcome measures by (1) investigating which of the three identified measures—the Home Support Needs Assessment, the Personal Care Participation Assessment and Resource Tool, and the Functional Autonomy Measurement System—best identifies meaningful changes in participation restrictions in daily life occupations required for community life; and (2) investigating the acceptability, usefulness, and feasibility of each measure to support inpatient practice.
Methods
Occupational therapists (n = 3) completed the three measures with patient participants (n = 12) at admission and discharge. Each occupational therapist participated in a semi-structured interview. Outcome measure responses were summarised statistically. Qualitative data were analysed using reflexive thematic analysis.
Findings
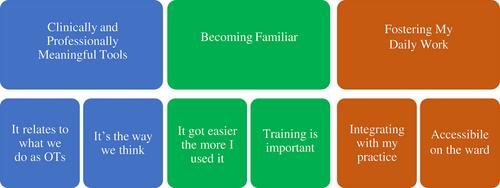
Total scores on all three measures changed significantly between admission and discharge (P < 0.002). Three themes reflected the occupational therapist participants' perceptions of the acceptability, usefulness, and feasibility of the outcome measures: ‘Clinically and Professionally Meaningful Tools’, ‘Becoming Familiar’, and ‘Fostering My Daily Work’.
Conclusion
Each measure demonstrated a meaningful change. Selection and successful implementation of an outcome measure depends on its local acceptability to occupational therapists and organisational practices. All three measures are promising tools to address a measurement gap in occupational therapy practice. Future research could embed one measure into practice using knowledge translation methods, with a large-scale evaluation of the value of occupational therapy.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


