Rectal sensitivity correlated with gastrointestinal-mediated glucose disposal, but not the incretin effect
Abstract
Objective
The mechanisms behind the diminished incretin effect in type 2 diabetes are uncertain, but impaired vagal transmission has been suggested. We aimed to investigate the association between the incretin effect and autonomic neuropathy, and the degree of dysglycaemia and duration of diabetes.
Design and Methods
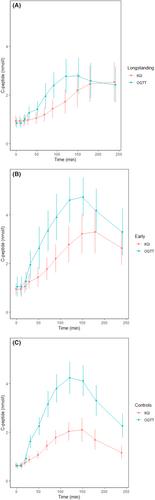
For a cross-sectional study, we included participants with either longstanding type 2 diabetes, recent onset, untreated diabetes and controls without diabetes matched for age, sex and body mass index. Autonomic nerve function was assessed with cardiovascular reflex tests, heart rate variability and sudomotor function. Visceral afferent nerves in the gut were tested performing rapid rectal balloon distention. An oral glucose tolerance test and an intravenous isoglycaemic glucose infusion were performed to calculate the incretin effect and gastrointestinal-mediated glucose disposal (GIGD).
Results
Sixty-five participants were recruited. Participants with diabetes had rectal hyposensitivity for earliest sensation (3.7 ± 1.1 kPa in longstanding, 4.0 ± 1.3 in early), compared to controls (3.0 ± 0.9 kPa), p = .005. Rectal hyposensitivity for earliest sensation was not associated with the incretin effect (rho = −0.204, p = .106), but an association was found with GIGD (rho −0.341, p = .005). Incretin effect and GIGD were correlated with all glucose values, HbA1c and duration of diabetes.
Conclusions
Rectal hyposensitivity was uncovered in both longstanding and early type 2 diabetes, and was not associated with the incretin effect, but with GIGD, implying a potential link between visceral neuropathy and gastrointestinal handling of glucose. Both the incretin effect and GIGD were associated with the degree of dysglycaemia and the duration of diabetes.
Previously Published
Some of the data have previously been published and presented as a poster on the American Diabetes Association 83rd Scientific Sessions: Meling et al; 1658-P: Rectal Hyposensitivity, a Potential Marker of Enteric Autonomic Nerve Dysfunction, Is Significantly Associated with Gastrointestinally Mediated Glucose Disposal in Persons with Type 2 Diabetes. Diabetes 20 June 2023; 72 (Supplement_1): 1658–P. https://doi.org/10.2337/db23-1658-P.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


