Calcium administration appears not to benefit acute pancreatitis patients with hypocalcemia
Abstract
Objective
Hypocalcemia occurs commonly among patients with acute pancreatitis (AP) in the intensive care unit (ICU). Calcium therapy could be used to correct hypocalcemia and maintain calcium levels, but its impact on the prognosis has not been demonstrated. Our study aimed to determine whether calcium therapy could benefit the multiple outcomes of AP patients with hypocalcemia.
Methods
We extracted 807 AP patients with hypocalcemia from the Beth Israel Deaconess Medical Center (MIMIC-IV) database and performed retrospective analyses. The outcomes were in-hospital, 28 days, ICU mortality, and the length of stay (LOS) in the hospital and ICU. We performed propensity matching (PSM) and inverse probability weighting (IPTW) to balance the baseline differences and conducted multivariate regression to investigate the impact of calcium therapy.
Results
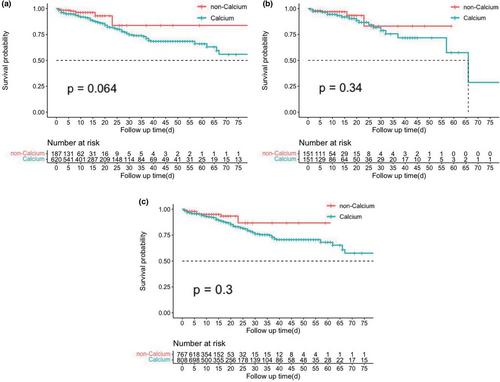
A total of 620 patients (76.8%) received calcium treatment (calcium group) during hospitalization, while 187 patients (non-calcium group) did not. Patients in the calcium group did not present significant survival differences between groups before and after matching. After including covariates, calcium administration had no association with patients' in-hospital (HR: 1.03, 95% Cl: 0.47–2.27, p = .942), 28 days and ICU mortality and was significantly associated with prolonged length of stay in the hospital (effect estimate: 6.18, 95% Cl: 3.27–9.09, p < .001) and ICU (effect estimate: 1.72, 95% Cl: 0.24–3.20, p < .001). Calcium therapy could not benefit patients in subgroups with exclusive parenteral infusion, early calcium therapy (<48 h), or various degrees of hypocalcemia.
Conclusion
AP patients with hypocalcemia could not benefit from calcium administration, which has no association with multiple mortality and is significantly associated with prolonged LOS in the hospital and ICU.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


