Psychometric Analysis of the Patient-Reported Hypoparathyroidism Symptom Diary Symptom Subscale Using Data from Two Clinical Trials.
IF 1.8
Q3 HEALTH CARE SCIENCES & SERVICES
Patient Related Outcome Measures
Pub Date : 2023-11-28
eCollection Date: 2023-01-01
DOI:10.2147/PROM.S414794
引用次数: 0
Abstract
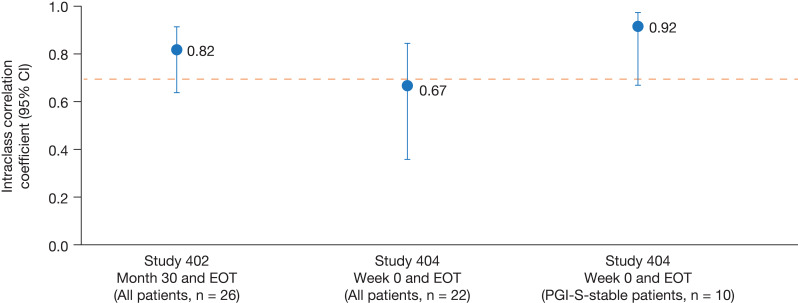
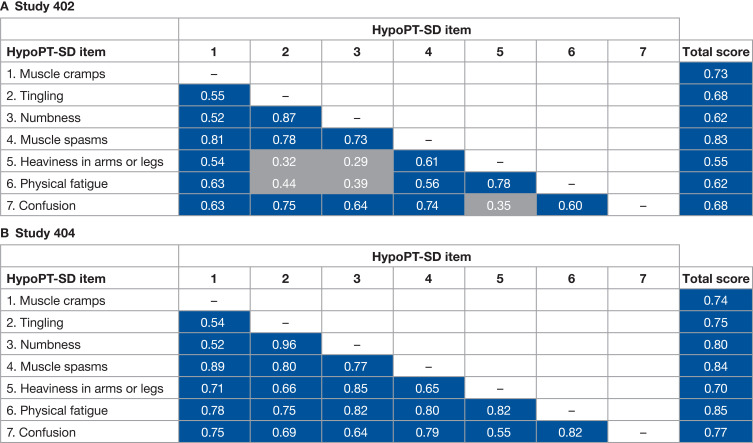
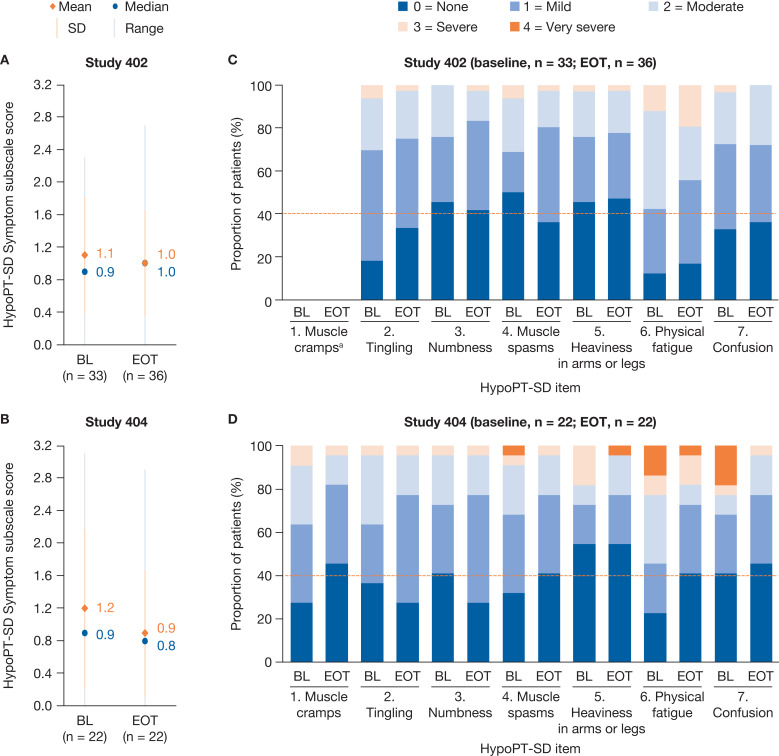
Purpose The hypoparathyroidism symptom diary (HypoPT-SD) is a disease-specific patient-reported outcome (PRO) tool comprising a 7-item symptom subscale, a 4-item impact subscale and 1-item anxiety, and sadness or depression components. This analysis assessed the psychometric properties of the HypoPT-SD symptom subscale scores using data from two open-label, single arm, Phase 4 studies (Study 402 and Study 404). Patients and Methods Eligible patients were aged 18 years or older with a confirmed diagnosis of hypoparathyroidism. All patients received recombinant human parathyroid hormone (1–84) during the analysis period. Scores were recorded at baseline, and at months 6, 30 and 36 (end of treatment [EOT]) in Study 402, and at baseline and week 52 (EOT) in Study 404. The structure of the HypoPT-SD Symptom subscale was analyzed by measuring correlations between pairs of item scores; internal consistency and reliability were evaluated using Cronbach’s coefficient α; test-retest reliability was assessed using intraclass correlation; and construct validity was determined by performing correlational analyses between scores recorded using the HypoPT-SD and those for other conceptually similar PRO tools. Results A total of 60 patients were included in the analysis. Inter-item pairwise correlations were strong for all but 5 of the item pairs analysed. Cronbach’s α values for the HypoPT-SD Symptom subscale were 0.88 using data from Study 402 and 0.92 using data from Study 404. In general, the HypoPT-SD Symptom subscale scores had moderate or strong correlations with scores recorded using PRO tools. Intraclass correlation coefficients exceeded 0.70 using test–retest data from all patients in Study 402 and from a subgroup of patients with stable disease from Study 404. Conclusion This analysis demonstrated the test-retest reliability, internal consistency and construct validity of the HypoPT-SD using data from longitudinal prospective studies and supports the use of the HypoPT-SD in future clinical studies.
患者报告的甲状旁腺功能减退症状日记症状亚量表的心理测量学分析,使用来自两个临床试验的数据。
目的:甲状旁腺功能减退症状日记(hyppt - sd)是一种疾病特异性的患者报告结果(PRO)工具,包括7项症状分量表、4项影响分量表和1项焦虑、悲伤或抑郁成分。本分析使用两个开放标签、单臂、4期研究(Study 402和Study 404)的数据评估了HypoPT-SD症状亚量表得分的心理测量特性。患者和方法:符合条件的患者年龄在18岁或以上,确诊为甲状旁腺功能减退。所有患者在分析期间均使用重组人甲状旁腺激素(1-84)。在研究402中记录基线、6个月、30个月和36个月(治疗结束[EOT])以及研究404中记录基线和52周(EOT)的评分。通过测量项目得分对之间的相关性来分析HypoPT-SD症状子量表的结构;采用Cronbach’s系数α评价内部一致性和信度;采用类内相关性评估重测信度;通过对使用HypoPT-SD和其他概念相似的PRO工具记录的分数进行相关性分析来确定结构效度。结果:共纳入60例患者。除了5个项目对外,其他项目对间的相关性都很强。hypoopt - sd症状子量表的Cronbach’s α值为0.88(研究402)和0.92(研究404)。一般来说,HypoPT-SD症状子量表得分与使用PRO工具记录的得分有中度或强相关性。研究402中所有患者和研究404中病情稳定的患者亚组的重测数据显示,类内相关系数超过0.70。结论:本分析利用纵向前瞻性研究数据证明了HypoPT-SD的重测信度、内部一致性和结构效度,支持HypoPT-SD在未来临床研究中的应用。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Patient Related Outcome Measures
HEALTH CARE SCIENCES & SERVICES-
自引率
4.80%
发文量
27
审稿时长
16 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


