Relapsing/remitting multiple sclerosis: A speculative model and its implications for a novel treatment
IF 4.1
4区 医学
Q2 IMMUNOLOGY
引用次数: 0
Abstract
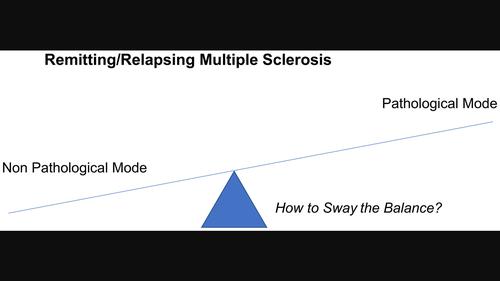
Abstract The clinical pattern in relapsing/remitting multiple sclerosis may be accounted for if an autoreactive immune response can transition back and forth between inflammatory, pathogenic, and non‐inflammatory, non‐pathogenic modes. Such ‘back‐and‐forth’ immune responses are rare. I speculate how such back‐and‐forth immune responses may arise. Understanding the nature of these different modes, and what controls their mutual transition, may help in designing strategies to favour the nonpathogenic mode, thus constituting treatment. Antigen dose is known to be critical in determining the class/subclass of primary immune responses. Observations have led us to suggest the level of antigen also similarly influences the class/subclass of on‐going immune responses. I propose the relapsing, inflammatory and the remitting modes are respectively sustained by relatively low and high amounts of the responsible autoantigens, as is the case, for example, for Th1 and Th2 responses to foreign antigens. In addition, I propose more self‐antigens are released during an inflammatory than during a remitting mode. The decrease in the amount of antigen released, as the response transitions from an inflammatory to a remitting mode, results in time in a decreased level of antigen and so the response again evolves towards the inflammatory mode. The inflammatory mode then leads to an increased release of antigen and so, in time, to remission. This model thus explains the transition between different modes. I outline non‐invasive, testable predictions of the hypothesis. If confirmed, it may be ethical to examine whether the non‐inflammatory mode can be sustained by administering myelin antigens during the remitting phase.
复发/缓解多发性硬化症:一个推测模型及其对一种新治疗方法的影响
如果自身反应性免疫反应能够在炎性、致病性和非炎性、非致病性模式之间来回转换,那么复发/缓解型多发性硬化症的临床模式可能得到解释。这种“来回”的免疫反应是罕见的。我推测这种来回的免疫反应是如何产生的。了解这些不同模式的本质,以及控制它们相互转换的因素,可能有助于设计有利于非致病性模式的策略,从而构成治疗。抗原剂量是决定原发性免疫反应类别/亚类别的关键因素。观察结果表明,抗原水平也同样影响正在进行的免疫反应的类别/亚类别。我认为复发,炎症和缓解模式分别由相对低和高的负责自身抗原维持,例如,对于Th1和Th2对外来抗原的反应。此外,我提出在炎症期间比缓解模式释放更多的自身抗原。当反应从炎症模式转变为缓解模式时,抗原释放量的减少导致抗原水平的下降,因此反应再次向炎症模式发展。然后,炎症模式导致抗原释放增加,从而及时缓解。因此,这个模型解释了不同模式之间的转换。我概述了该假设的非侵入性、可测试的预测。如果得到证实,检验在缓解期给予髓鞘抗原是否能维持非炎症模式可能是合乎伦理的。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
7.70
自引率
5.40%
发文量
109
审稿时长
1 months
期刊介绍:
This peer-reviewed international journal publishes original articles and reviews on all aspects of basic, translational and clinical immunology. The journal aims to provide high quality service to authors, and high quality articles for readers.
The journal accepts for publication material from investigators all over the world, which makes a significant contribution to basic, translational and clinical immunology.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


