Analysis of the incidence of falls and related factors in elderly patients based on comprehensive geriatric assessment
Abstract
Objective
To investigate the incidence of falls in elderly aged 65 years and above among outpatients and inpatients, and to analyze its related factors and identify prevention strategies.
Methods
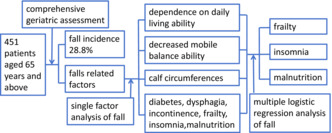
A retrospective analysis was conducted on 451 patients aged 65 years and above who received comprehensive geriatric assessment in outpatients and inpatients from the Department of Geriatrics in the Second Xiangya Hospital from March 2021 to March 2022. According to whether there had been at least one fall in the past year, the patients were divided into a fall group and a non-fall group. Data were collected from the We-Chat applet of comprehensive geriatric assessment. A t test and chi-square test were performed to compare the difference between the two groups. Logistic regression analysis was then conducted to identify factors associated with falls.
Results
(1) The incidence of falls among the outpatient and inpatient was 28.8%. (2) The rate of light, moderate, and heavy dependence on daily living ability and decreased mobile balance ability were higher in the fall group than those in the non-fall group. The average calf circumference in the fall group was significantly lower than that in the non-fall group. (3) The prevalence of diabetes and eye diseases in the fall group was significantly higher than that in the non-fall group. (4) The percentage of insomnia and suspicious insomnia cases in the fall group was higher than that in the non-fall group. The mean scores for dysphagia, frailty, and incontinence were higher and the mean malnutrition score was lower in the fall group than in the non-fall group. (5) Multiple logistic regression analysis showed that frailty, insomnia, and malnutrition were independent influencing factors of fall (OR = 1.955, 1.652, 10.719, P = 0.044, 0.041, 0.025, respectively).
Conclusions
The incidence of falls among outpatients and inpatients aged 65 years and above is high. Frailty, insomnia, and malnutrition are the main factors influencing falls in these patients.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


