Call for standardization in assessment and reporting of muscle and adipose change using computed tomography analysis in oncology: A scoping review
IF 9.1
1区 医学
引用次数: 0
Abstract
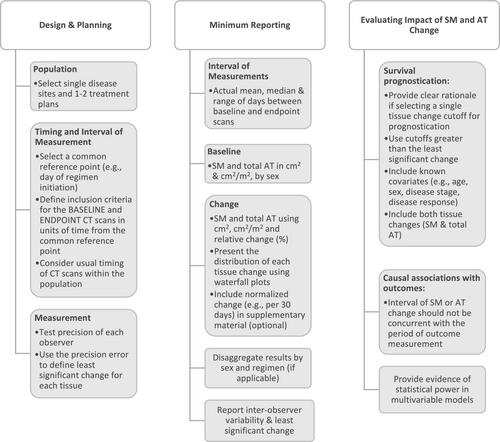
Investigators are increasingly measuring skeletal muscle (SM) and adipose tissue (AT) change during cancer treatment to understand impact on patient outcomes. Recent meta‐analyses have reported high heterogeneity in this literature, representing uncertainty in the resulting estimates. Using the setting of palliative‐intent chemotherapy as an exemplar, we aimed to systematically summarize the sources of variability among studies evaluating SM and AT change during cancer treatment and propose standards for future studies to enable reliable meta‐analysis. Studies that measured computed tomography‐defined SM and/or AT change in adult patients during palliative‐intent chemotherapy for solid tumours were included, with no date or geographical limiters. Of 2496 publications screened by abstract/title, 83 were reviewed in full text and 38 included for extraction, representing 34 unique cohorts across 8 tumour sites. The timing of baseline measurement was frequently defined as prior to treatment, while endpoint timing ranged from 6 weeks after treatment start to time of progression. Fewer than 50% specified the actual time interval between measurements. Measurement error was infrequently discussed (8/34). A single metric (cm2/m2, cm2 or %) was used to describe SM change in 18/34 cohorts, while multiple metrics were presented for 10/34 and no descriptive metrics for 6/34. AT change metrics and sex‐specific reporting were available for 10/34 cohorts. Associations between SM loss and overall survival were evaluated in 24 publications, with classification of SM loss ranging from any loss to >14% loss over variable time intervals. Age and sex were the most common covariates, with disease response in 50% of models. Despite a wealth of data and effort, heterogeneity in study design, reporting and statistical analysis hinders evidence synthesis regarding the severity and outcomes of SM and AT change during cancer treatment. Proposed standards for study design include selection of homogenous cohorts, clear definition of baseline/endpoint timing and attention to measurement error. Standard reporting should include baseline SM and AT by sex, actual scan interval, SM and AT change using multiple metrics and visualization of the range of change observed. Reporting by sex would advance understanding of sexual dimorphism in SM and AT change. Evaluating the impact of tissue change on outcomes requires adjustment for relevant covariates and concurrent disease response. Adoption of these standards by researchers and publishers would alter the current paradigm to enable meta‐analysis of future studies and move the field towards meaningful application of SM and AT change to clinical care.
呼吁在肿瘤学中使用计算机断层扫描分析对肌肉和脂肪变化的评估和报告进行标准化:范围界定综述。
研究人员越来越多地测量癌症治疗期间骨骼肌(SM)和脂肪组织(AT)的变化,以了解对患者结果的影响。最近的荟萃分析报告了该文献中的高度异质性,代表了由此产生的估计的不确定性。以缓解期化疗为例,我们旨在系统总结评估癌症治疗期间SM和AT变化的研究的变异性来源,并为未来的研究提出标准,以实现可靠的荟萃分析。包括测量计算机断层扫描定义的成年患者在实体瘤姑息性化疗期间SM和/或AT变化的研究,没有日期或地理限制。在2496篇按摘要/标题筛选的出版物中,83篇为全文综述,38篇为摘录,代表了8个肿瘤部位的34个独特队列。基线测量的时间通常定义为治疗前,而终点时间从治疗开始后6周到进展时间不等。少于50%的人指定了测量之间的实际时间间隔。很少讨论测量误差(8/34)。在18/34队列中,使用单一指标(cm2/m2、cm2或%)来描述SM变化,而在10/34队列中使用了多个指标,在6/34队列中没有使用描述性指标。10/34队列的AT变化指标和性别特异性报告可用。在24篇出版物中评估了SM损失与总生存率之间的相关性,SM损失的分类从任何损失到变化时间间隔内损失>14%不等。年龄和性别是最常见的协变量,50%的模型有疾病反应。尽管有丰富的数据和努力,但研究设计、报告和统计分析的异质性阻碍了关于癌症治疗期间SM和AT变化的严重程度和结果的证据综合。研究设计的拟议标准包括同质队列的选择、基线/终点时间的明确定义以及对测量误差的关注。标准报告应包括按性别、实际扫描间隔、使用多种指标的SM和AT基线变化以及观察到的变化范围的可视化。按性别报告将促进对SM和AT变化中两性异形的理解。评估组织变化对结果的影响需要对相关协变量和并发疾病反应进行调整。研究人员和出版商采用这些标准将改变当前的范式,使未来的研究能够进行荟萃分析,并推动该领域将SM和AT变化有意义地应用于临床护理。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Journal of Cachexia, Sarcopenia and Muscle
Medicine-Orthopedics and Sports Medicine
自引率
12.40%
发文量
0
期刊介绍:
The Journal of Cachexia, Sarcopenia, and Muscle is a prestigious, peer-reviewed international publication committed to disseminating research and clinical insights pertaining to cachexia, sarcopenia, body composition, and the physiological and pathophysiological alterations occurring throughout the lifespan and in various illnesses across the spectrum of life sciences. This journal serves as a valuable resource for physicians, biochemists, biologists, dieticians, pharmacologists, and students alike.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


