Role of Blood–Brain Barrier Dysfunction in Delirium following Non-cardiac Surgery in Older Adults
Abstract
Objective
Although animal models suggest a role for blood–brain barrier dysfunction in postoperative delirium-like behavior, its role in postoperative delirium and postoperative recovery in humans is unclear. Thus, we evaluated the role of blood–brain barrier dysfunction in postoperative delirium and hospital length of stay among older surgery patients.
Methods
Cognitive testing, delirium assessment, and cerebrospinal fluid and blood sampling were prospectively performed before and after non-cardiac, non-neurologic surgery. Blood–brain barrier dysfunction was assessed using the cerebrospinal fluid-to-plasma albumin ratio (CPAR).
Results
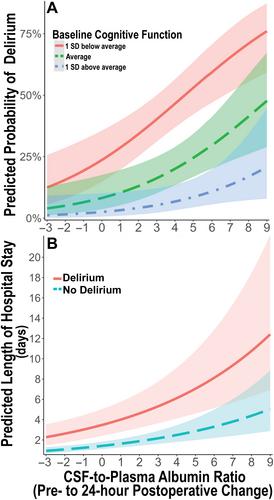
Of 207 patients (median age = 68 years, 45% female) with complete CPAR and delirium data, 26 (12.6%) developed postoperative delirium. Overall, CPAR increased from before to 24 hours after surgery (median change = 0.28, interquartile range [IQR] = −0.48 to 1.24, Wilcoxon p = 0.001). Preoperative to 24 hours postoperative change in CPAR was greater among patients who developed delirium versus those who did not (median [IQR] = 1.31 [0.004 to 2.34] vs 0.19 [−0.55 to 1.08], p = 0.003). In a multivariable model adjusting for age, baseline cognition, and surgery type, preoperative to 24 hours postoperative change in CPAR was independently associated with delirium occurrence (per CPAR increase of 1, odds ratio = 1.30, 95% confidence interval [CI] = 1.03–1.63, p = 0.026) and increased hospital length of stay (incidence rate ratio = 1.15, 95% CI = 1.09–1.22, p < 0.001).
Interpretation
Postoperative increases in blood–brain barrier permeability are independently associated with increased delirium rates and postoperative hospital length of stay. Although these findings do not establish causality, studies are warranted to determine whether interventions to reduce postoperative blood–brain barrier dysfunction would reduce postoperative delirium rates and hospital length of stay. ANN NEUROL 2023;94:1024–1035

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


