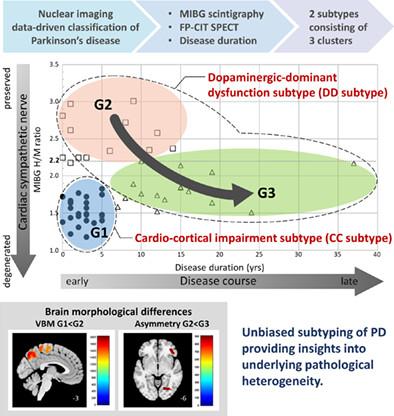
Nuclear Imaging Data-Driven Classification of Parkinson's Disease
Abstract
BACKGROUND
Parkinson's disease (PD) is a heterogeneous neurodegenerative disorder characterized by motor and nonmotor symptoms. Several features have prognostic importance and have been used as key indicators for identifying clinical subtypes. However, the symptom-based classification approach has limitations with respect to the stability of the obtained subtypes.
OBJECTIVES
The purpose of this study was to identify subtypes of PD using nuclear imaging biomarkers targeting the cardiac sympathetic nervous and nigro-striatal systems and to compare patterns of cortical morphological change among obtained subtypes.
METHODS
We performed unbiased hierarchical cluster analysis using 123I-metaiodobenzylguanidine cardiac scintigraphy and 123I-N-(3-fluoropropyl)-2β-carbomethoxy-3β-(4-iodophenyl) nortropane single photon emission computed tomography data for 56 patients with PD. We compared clinical characteristics and the patterns of cortical atrophy in the obtained clusters.
RESULTS
Three clusters were identified and showed distinct characteristics in onset ages and dopamine-replacement therapy and deep brain stimulation requirements. According to the characteristics, clusters were classified into two subtypes, namely, “cardio-cortical impairment (CC)” and “dopaminergic-dominant dysfunction (DD)” subtype. The three clusters were named according to subtype and time since onset in which 14 patients were classified as “early DD,” 25 as “advanced DD,” and 17 as “early CC.” Compared with the early DD subtype, the early CC subtype showed parietal-dominant diffuse cortical atrophy and the advanced DD subtype showed left-side predominant mild cortical atrophy.
CONCLUSIONS
Nuclear imaging biomarker–based classification can be used to identify clinically and pathologically relevant PD subtypes with distinct disease trajectories. © 2023 International Parkinson and Movement Disorder Society.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


