Association between hemoglobin glycation index and non-alcoholic fatty liver disease in the patients with type 2 diabetes mellitus
Abstract
Aims/Introduction
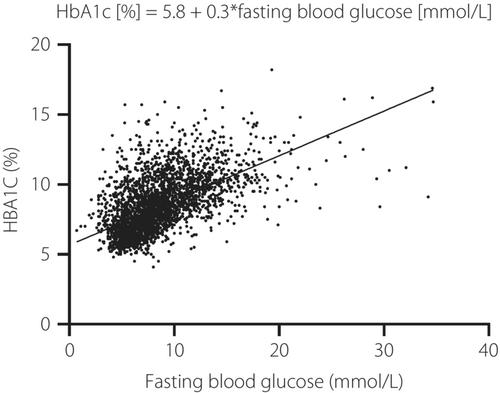
The hemoglobin glycation index (HGI) represent the disparity between actual glycated hemoglobin measurements and predicted HbA1c. It serves as a proxy for the degree of non-enzymatic glycation of hemoglobin, which has been found to be positively correlated with diabetic comorbidities. In this study, we investigated the relationship between HGI and non-alcoholic fatty liver disease (NAFLD), along with other relevant biological markers in patients with diabetes.
Materials and Methods
This cross-sectional study consisted of 3,191 adults diagnosed with type 2 diabetes mellitus. We calculated the predicted glycated hemoglobin levels based on fasting blood glucose levels. Multivariate binary logistic regression analysis was conducted to examine the correlation between the HGI and NAFLD. Hepatic steatosis was diagnosed using ultrasonography.
Results
Among all participants, 1,784 (55.91%) were diagnosed with NAFLD. Participants with confirmed NAFLD showed elevated body mass index, diastolic blood pressure, liver enzyme, total cholesterol, triglyceride, low-density lipoprotein and uric acid levels compared with those without NAFLD. In the unadjusted model, participants in the last tertile of HGI were 1.40-fold more likely to develop NAFLD than those in the first tertile (95% confidence interval 1.18–1.66; P < 0.001). In the fully adjusted model, those in the last tertile of HGI had a 39% increased risk of liver steatosis compared with confidence interval in the first tertile of HGI (95% confidence interval 1.12–1.74; P < 0.001).
Conclusions
A higher HGI suggests an elevated risk of developing NAFLD in patients with type 2 diabetes.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


