The estimated health impact of alcohol interventions in New Zealand: A modelling study
Abstract
Aims
To estimate the health impacts of key modelled alcohol interventions among Māori (indigenous peoples) and non-Māori in New Zealand (NZ).
Design
Multi-stage life-table intervention modelling study. We modelled two scenarios: (1) business-as-usual (BAU); and (2) an intervention package scenario that included a 50% alcohol tax increase, outlet density reduction from 63 to five outlets per 100 000 people, outlet hours reduction from 112 to 50 per week and a complete ban on all forms of alcohol marketing.
Setting and participants
The model’s population replicates the 2018 NZ population by ethnicity (Māori/non-Māori), age and sex.
Measurements
Alcohol consumption was estimated using nationally representative survey data combined with sales data and corrected for tourist and unrecorded consumption. Disease incidence, prevalence and mortality were calculated using Ministry of Health data. We used dose–response relationships between alcohol and illness from the 2016 Global Burden of Disease study and calculated disability rates for each illness. Changes in consumption were based on the following effect sizes: total intervention package [−30.3%, standard deviation (SD) = 0.02); tax (−7.60%, SD = 0.01); outlet density (−8.64%, SD = 0.01); outlet hours (−9.24%, SD = 0.01); and marketing (−8.98%, SD = 0.02). We measured health gain using health-adjusted life years (HALYs) and life expectancy.
Findings
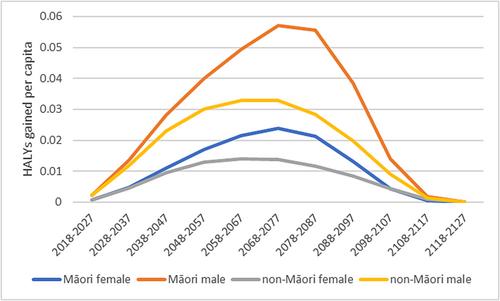
Compared with the BAU scenario, the total alcohol intervention package resulted in 726 000 [95% uncertainty interval (UI) = 492 000–913 000] HALYs gained during the life-time of the modelled population. Māori experienced greater HALY gains compared with non-Māori (0.21, 95% UI = 0.14–0.26 and 0.16, 95% UI = 0.11–0.20, respectively). When modelled individually, each alcohol intervention within the intervention package produced similar health gains (~200 000 HALYs per intervention) owing to the similar effect sizes.
Conclusions
Modelled interventions for increased alcohol tax, reduced availability of alcohol and a ban on alcohol marketing among Māori and non-Māori in New Zealand (NZ) suggest substantial population-wide health gains and reduced health inequities between Māori and non-Māori.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


