Favourable cognitive changes observed with metabolic improvements in a patient with severe mental illness.
IF 4.1
2区 医学
Q2 NEUROSCIENCES
Journal of Psychiatry & Neuroscience
Pub Date : 2023-09-06
Print Date: 2023-09-01
DOI:10.1503/jpn.230052
引用次数: 1
Abstract
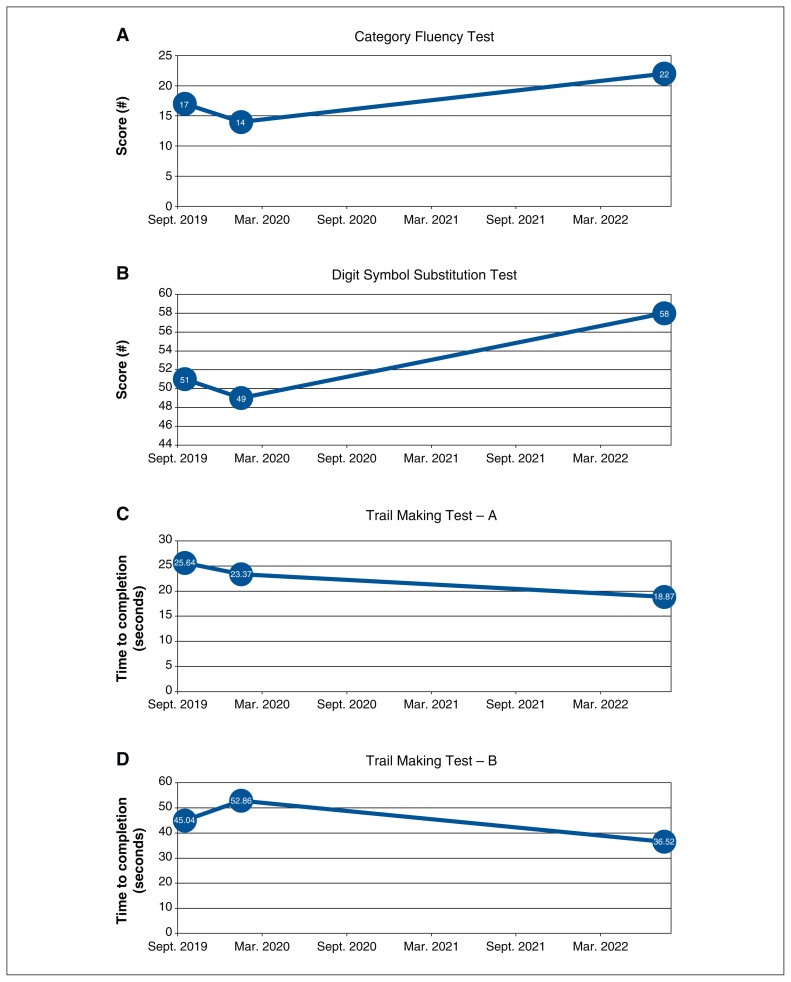
A 41-year-old unemployed woman with longstanding major depressive and social anxiety disorder was referred to the Metabolic Clinic at the Centre for Addiction and Mental Health for weight gain concerns. She had maintained a weight of about 54 kg during adulthood, until she gained 41 kg over a period of 1.5 years during the course of several antipsychotic and antidepressant trials. The patient’s current psychotropics and metabolically active medications included quetiapine (300 mg/d at bedtime), ketamine (250 mg, inhaled every 3 days), zopiclone (22.5 mg/d at bedtime), baclofen (55 mg/d), lorazepam (2 mg at bedtime) and sumatriptan (100 mg/d as needed). She preferred to continue quetiapine given the stability of her psychiatric symptoms. Her psychotropic medications were managed by her treating psychiatrist. The patient weighed 95.6 kg at the time of consultation, translating to class III obesity and a body mass index (BMI) of 42.5 kg/m2. She met criteria for abdominal obesity, with a waist circumference of 108 cm. Bloodwork showed evidence of metabolic dysfunction, with elevated levels of fasting glucose (6.4 mmol/L), fast ing insulin (297 pmol/L), low-density lipoprotein (LDL) cholesterol (2.93 mmol/L), total cholesterol (5.87 mmol/L) and triglycerides (2.35 mmol/L). High-density lipoprotein (HDL) cholesterol was 1.87 mmol/L. We recommended metformin, a well-tolerated antihyperglycemic agent that has the strongest evidence of benefit for antipsychoticinduced weight gain.1 We initiated 500 mg/d and titrated the dose to 2500 mg/d. The patient concurrently implemented lifestyle modifications, including improved diet and increased physical activity, walking up to 5 times per week for up to 2 hours each time. With metformin and the lifestyle changes combined, the patient lost about 45 kg over 3 years. No adverse effects were reported, and her weight loss was gradual at 1–3 kg per month (Table 1). She weighed 49.2 kg at her most recent visit, and both her BMI and waist circumference normalized to 21.9 kg/m2 and 65 cm, respectively. Improvements in other metabolic par ameters were observed, including reduced triglycerides (down to 1.26 mmol/L), fasting glucose (5.6 mmol/L), and insulin (61 pmol/L) The information in this column is not intended as a definitive treatment strategy but as a suggested approach for clinicians treating patients with similar histories. Individual cases may vary and should be evaluated carefully before treatment is provided. The patient described in this column gave informed consent for its publication. Psychopharmacology for the Clinician
在一名患有严重精神疾病的患者中,随着代谢的改善,观察到了有利的认知变化。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
6.80
自引率
2.30%
发文量
51
审稿时长
2 months
期刊介绍:
The Journal of Psychiatry & Neuroscience publishes papers at the intersection of psychiatry and neuroscience that advance our understanding of the neural mechanisms involved in the etiology and treatment of psychiatric disorders. This includes studies on patients with psychiatric disorders, healthy humans, and experimental animals as well as studies in vitro. Original research articles, including clinical trials with a mechanistic component, and review papers will be considered.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


