Relationship between baseline electrocardiographic measurements and outcomes in patients with high-risk heart failure: Insights from the VerICiguaT Global Study in Subjects with Heart Failure with Reduced Ejection Fraction (VICTORIA) trial
Abstract
Aims
Whether electrocardiographic (ECG) measurements predict mortality in chronic heart failure with reduced ejection fraction (HFrEF) is unknown.
Methods and results
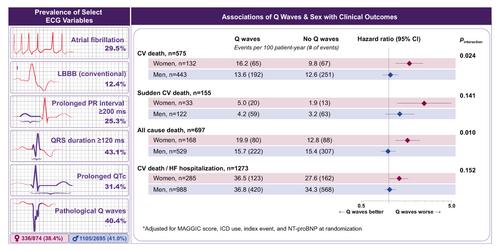
We studied 4880 patients from the Vericiguat Global Study in Subjects with Heart Failure with Reduced Ejection Fraction (VICTORIA) trial with a baseline 12-lead ECG. Associations between ECG measurements and mortality were estimated as hazard ratios (HR) and adjusted for the Meta-Analysis Global Group in Chronic Heart Failure (MAGGIC) risk score, N-terminal pro-B-type natriuretic peptide, and index event. Select interactions between ECG measurements, patient characteristics and mortality were examined. Over a median of 10.8 months, there were 824 cardiovascular (CV) deaths (214 sudden) and 1005 all-cause deaths. Median age was 68 years (interquartile range [IQR] 60–76), 24% were women, median ejection fraction was 30% (IQR 23–35), 41% had New York Heart Association class III/IV, and median MAGGIC score was 24 (IQR 19–28). After multivariable adjustment, significant associations existed between heart rate (per 5 bpm: HR 1.02), QRS duration (per 10 ms: HR 1.02), absence of left ventricular hypertrophy (HR 0.64) and CV death, and similarly so with all-cause death (HR 1.02; HR 1.02; HR 0.61, respectively). Contiguous pathologic Q waves were significantly associated with sudden death (HR 1.46), and right ventricular hypertrophy with all-cause death (HR 1.44). The only sex-based interaction observed was for pathologic Q waves on CV (men: HR 1.05; women: HR 1.64, pinteraction = 0.024) and all-cause death (men: HR 0.99; women: HR 1.57; pinteraction = 0.010). Whereas sudden death doubled in females, it did not differ among males (male: HR 1.25, 95% confidence interval [CI] 0.87–1.79; female: HR 2.50, 95% CI 1.23–5.06; pinteraction = 0.141).
Conclusion
Routine ECG measurements provide additional prognostication of mortality in high-risk HFrEF patients, particularly in women with contiguous pathologic Q waves.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


