基于苯巴比妥的ICU酒精戒断综合征治疗方案:实施前后研究
引用次数: 1
摘要
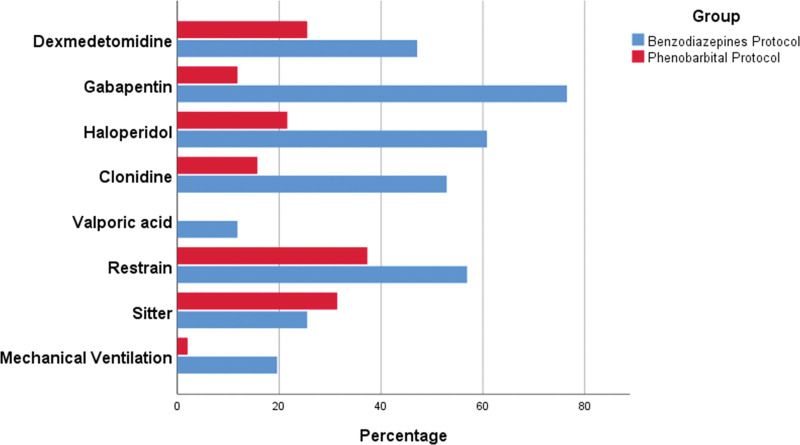
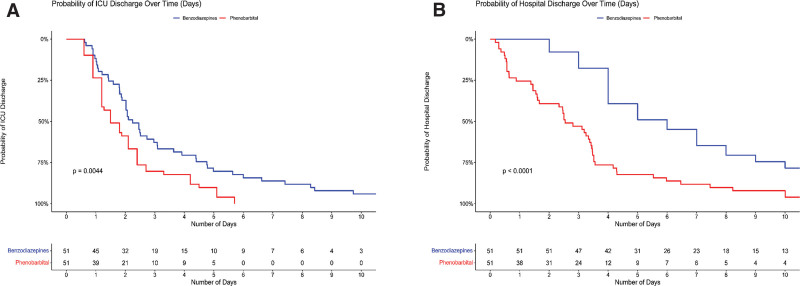
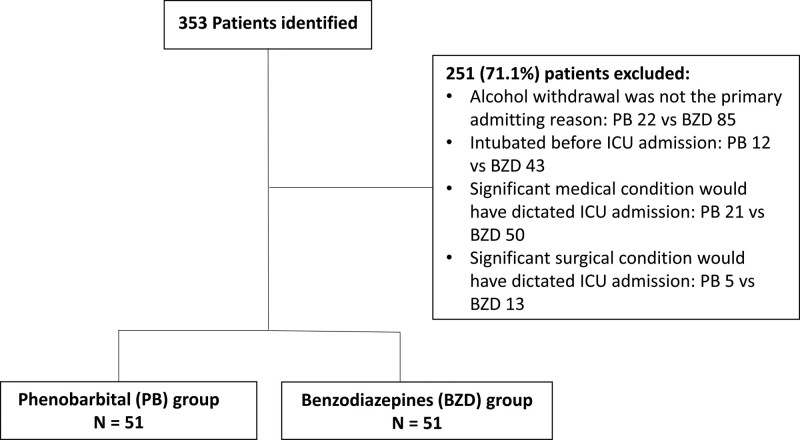
我们比较了以苯二氮卓类药物(BZD)为基础的方案治疗重症重症患者AWS的疗效和安全性。设计:单中心,前后协议实施研究。设置:设置在三级学术医疗中心的40个床位的MICU。患者:我们纳入了所有最初诊断为AWS的MICU患者。干预措施:静脉注射PB 260 mg,然后根据需要每15-30分钟给药130 mg,每次给药至理想体重15 mg/kg,而不是逐渐增加BZD剂量,以达到临床研究所戒断评估酒精量表修订评分低于10分。测量和主要结果:ICU和住院时间(LOS),以及安全措施是研究的主要结果。共纳入102例患者,51例在PB组,51例在BZD组。两组的基线临床特征无差异。两组各有一半患者入院时伴有震颤性谵妄。使用基于pbp的方案可使ICU LOS中位数降低35% (1.5 d[四分位数间距,1.2-2.4 d] vs 2.3 d [1.4-4.8 d];p = 0.009),住院LOS降低50% (3 d [2.7-4 d] vs 6 d [4-10 d];P < 0.001)。在调整合并症和临床因素后,PB方案使ICU的LOS天数减少了40% (95% CI;25.8 - -53.5%)。PB组需要较少的辅助药物来控制症状(0.7 [0.5-1]vs 2.5 [2-3]);P < 0.001),插管需求减少(1/51 [2%]vs 10/10 [19.6%];P = 0.023)和较少的身体约束需求(19/51 [37.3%]vs 29/51 [56.9%];p = 0.047),与BZD组比较。结论:短期内快速递增剂量的PB治疗方案是治疗MICU患者AWS的有效且安全的替代方案。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Phenobarbital-Based Protocol for Alcohol Withdrawal Syndrome in a Medical ICU: Pre-Post Implementation Study.
OBJECTIVES: We assessed the efficacy and safety of PB compared with benzodiazepine (BZD)-based protocols in treating AWS in MICU. DESIGN: Single-center, pre-post protocol implementation study. SETTING: The setting is a forty-bed MICU in a tertiary-level academic medical center. PATIENTS: We included all patients admitted to the MICU with a primary diagnosis of AWS. INTERVENTIONS: Intravenous PB 260 mg followed by 130-mg doses every 15–30 minutes as needed up to 15 mg/kg of ideal body weight versus escalating doses of BZD, to achieve a Clinical Institute Withdrawal Assessment Alcohol Scale-Revised score less than 10. MEASUREMENTS AND MAIN RESULTS: ICU and hospital length of stay (LOS), in addition to safety measures were the main outcomes of the study. A total of 102 patients were included, 51 in the PB arm and 51 in the BZD arm. There were no differences in baseline clinical characteristics. Half the patients in each group were admitted with delirium tremens. The use of PB-based protocol was associated with 35% reduction in median ICU LOS (1.5 d [interquartile range, 1.2–2.4 d] vs 2.3 d [1.4–4.8 d]; p = 0.009) and 50% reduction in hospital LOS (3 d [2.7–4 d] vs 6 d [4–10 d]; p < 0.001). After adjustment for comorbidities and clinical factors, PB protocol decreased ICU LOS days by 40% (95% CI; 25.8–53.5%). PB group required fewer adjunctive medications to control symptoms (0.7 [0.5–1] vs 2.5 [2–3]; p < 0.001), less need for intubation (1/51 [2%] vs 10/10 [19.6%]; p = 0.023) and less need for physical restraint (19/51 [37.3%] vs 29/51 [56.9%]; p = 0.047), compared with the BZD group. CONCLUSIONS: A protocol utilizing rapidly escalating doses of PB over a short period is an effective and safe alternative to BZD in treating AWS in MICU.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


