不是所有溃疡都是克罗恩病。
IF 1
Q4 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
摘要
本文章由计算机程序翻译,如有差异,请以英文原文为准。
Not Everything That Ulcerates Is Crohn's Disease.
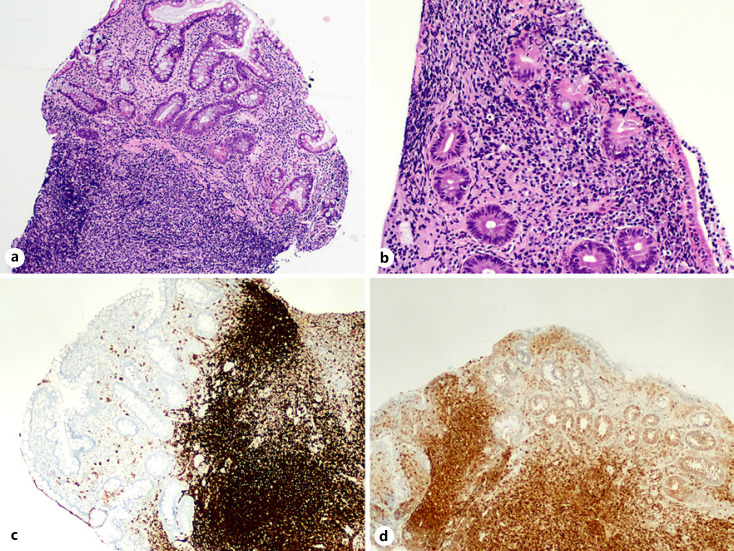
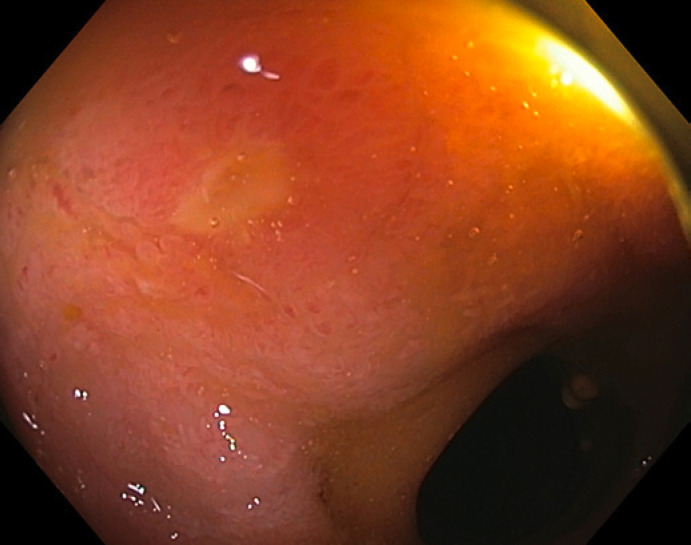
A 41-year-old male with a history of Crohn’s disease (CD) with penetrating phenotype (A2L2B3p, Montreal Classification), who was diagnosed aged 17 years and had started treatment with infliximab monotherapy at 30 years old, had been on clinical, imagiological, and endoscopic remission for the previous 2 years. On follow-up ileocolonoscopy with the purpose of considering stopping biological treatment (per the patient’s wishes), only 2 superficial ulcers in the sigmoid colon and 3 small erosions in the terminal ileum (shown in Fig. 1) were detected. Histological examination of the ileum erosions demonstrated an infiltrate of atypical lymphoepithelial cells, CD20 positive and CD5, CD23, CD10, and cyclinD1 negative, compatible with a marginal zone B-cell lymphoma of the mucosal-associated lymphoid tissue (MALT; shown in Fig. 2). Immunoglobulin deposition was not identified in this tissue. Cervico-thoraco-abdominopelvic computed tomography and magnetic resonance bowel enterography were unremarkable. The histological specimens were analyzed by two different pathologists with expertise in hematopathology. Serum lactate dehydrogenase, β2-microglobulin, and immunoglobulin levels were normal. Hepatitis C virus antibodies and DNA of Campylobacter jejuni on ileum tissue were negative. Staging was complete as a MALTlymphoma Galian stage A and Lugano stage I. A 6-month course of antibiotic therapy with combined metronidazole and ampicillin was proposed after consultation with Hematology. As the patient was in clinical remission and the endoscopic activity was residual, biologic therapy was suspended due to an unfavorable risk/benefit. Unfortunately, CD recurred clinically and endoscopically so vedolizumab was started after endoscopic and histologic documentation of MALT remission (1 year after diagnosis, 6 months after antibiotics). Due to a primary non-response, the patient was swapped to ustekinumab and is currently in clinical remission, with a further endoscopic evaluation at 6–9 months.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

GE Portuguese Journal of Gastroenterology
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
1.60
自引率
11.10%
发文量
62
审稿时长
21 weeks
期刊介绍:
The ''GE Portuguese Journal of Gastroenterology'' (formerly Jornal Português de Gastrenterologia), founded in 1994, is the official publication of Sociedade Portuguesa de Gastrenterologia (Portuguese Society of Gastroenterology), Sociedade Portuguesa de Endoscopia Digestiva (Portuguese Society of Digestive Endoscopy) and Associação Portuguesa para o Estudo do Fígado (Portuguese Association for the Study of the Liver). The journal publishes clinical and basic research articles on Gastroenterology, Digestive Endoscopy, Hepatology and related topics. Review articles, clinical case studies, images, letters to the editor and other articles such as recommendations or papers on gastroenterology clinical practice are also considered. Only articles written in English are accepted.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


