三个N2站的采样是否应该是I期癌症根治性切除的质量指标?
IF 4.9
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
Journal of Thoracic and Cardiovascular Surgery
Pub Date : 2024-11-01
DOI:10.1016/j.jtcvs.2023.10.058
引用次数: 0
摘要
目标:2022年,ACS癌症委员会(CoC)发布了标准5.8质量指标,用于需要从3个N2站进行淋巴结切除的癌症治疗切除。在本报告中,我们比较了I期非小细胞肺癌切除3个N2站和2个N2站后的肿瘤学结果。方法:从2011-2020年对单一机构数据库进行回顾性审查,以确定临床I期非大细胞肺癌患者。有癌症、类癌、磨玻璃病变病史的患者。结果:581例患者被识别,并根据检查的N2站数分为两组;A组检查了2个N2站(364名患者),B组检查了3个以上的N2站(217名患者)。两组之间的基线人口统计学和临床特征相似。在A组中,8.2%(30/364)和5.2%(19/364)的患者存在N1和N2阳性淋巴结,而B组分别为7.4%(16/217)和5.5%(12/217)。5年OS和DFS在A组分别为89%和74%,而在B组则分别为88%和78%。复发发生在A组56例(15.4%)(6.6%局部和8.8%远处)和B组29例(13.4%)(5.1%局部和8.3%远处;p=0.73)。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Should sampling of three N2 stations be a quality metric for curative resection of stage I lung cancer?
Objective
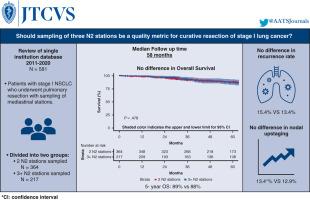
In 2022, the American College of Surgeons Commission on Cancer issued standard 5.8 quality metric for curative lung cancer resections requiring nodal resection from 3 N2 stations. In this report, we compare oncologic outcomes after resection of 3 N2 stations versus 2 N2 stations in stage I non–small cell lung cancer.
Methods
A retrospective review from a single institution database was conducted from 2011 to 2020 to identify patients with clinical stage I non–small cell lung cancer. Patients with a history of lung cancer, carcinoid tumors, and ground-glass lesions less than 50% solid component were excluded. The primary outcome was overall survival. Secondary outcomes included disease-free survival, recurrence patterns, and nodal upstaging.
Results
A total of 581 patients were identified and divided into 2 groups based on the number of N2 stations examined: Group A had 2 N2 stations examined (364 patients), and group B had 3 or more N2 stations examined (217 patients). Baseline demographic and clinical characteristics were similar between groups. In group A, N1 and N2 positive nodal stations were present in 8.2% (30/364) and 5.2% (19/364) of patients versus 7.4% (16/217) and 5.5% (12/217), respectively, in group B. Five-year overall survival and disease-free survival were 89% and 74% in group A versus 88% and 78% in group B, respectively. Recurrence occurred in 56 patients (15.4%) in group A (6.6% local and 8.8% distant) and 29 patients (13.4%) in group B (5.1% local and 8.3% distant; P = .73).
Conclusions
There was no significant difference in oncological outcomes in stage I non–small cell lung cancer resections that included 2 N2 stations compared with at least 3 N2 stations examined.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
11.20
自引率
10.00%
发文量
1079
审稿时长
68 days
期刊介绍:
The Journal of Thoracic and Cardiovascular Surgery presents original, peer-reviewed articles on diseases of the heart, great vessels, lungs and thorax with emphasis on surgical interventions. An official publication of The American Association for Thoracic Surgery and The Western Thoracic Surgical Association, the Journal focuses on techniques and developments in acquired cardiac surgery, congenital cardiac repair, thoracic procedures, heart and lung transplantation, mechanical circulatory support and other procedures.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


