平均血小板体积与MDD关系的回顾性研究。
引用次数: 38
摘要
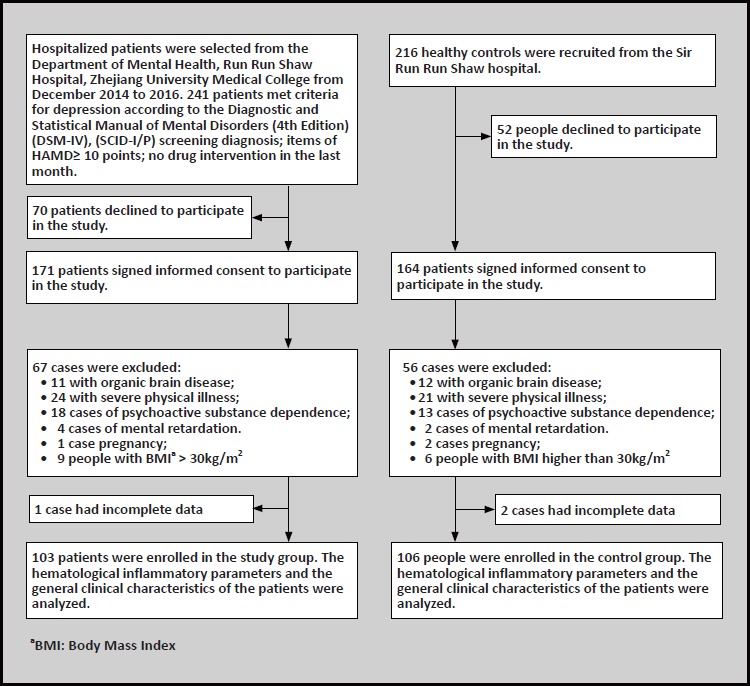
背景:大量研究结果表明,重度抑郁症(MDD)与慢性低度炎症有关,但其潜在机制尚不清楚。目的:比较MDD患者与健康对照者的血细胞分析结果,探讨其作为MDD免疫炎症指标的潜在价值,尤其是血小板平均体积。方法:招募年龄、性别匹配的重度抑郁症患者103例,健康对照106例。我们采集了两组的外周血样本并收集了基本数据。组间正态分布数据(年龄、体重指数、淋巴细胞计数、白细胞计数、红细胞计数、红细胞比容、血小板计数、平均红细胞体积)比较采用单t检验;对于非正态分布数据(中性粒细胞计数、中性粒细胞计数、血小板/淋巴细胞比值、血红蛋白、红细胞分布宽度、平均血小板体积、平均血红蛋白浓度、平均血红蛋白和血小板分布宽度)的比较,我们采用Mann-Whitney u检验。结果:与健康对照组相比,MDD组白细胞计数(F=0.443, p=0.004)、血小板密度(F=8.3, pZ=-6.063, pZ=-5.062)、血小板/淋巴细胞比值(Z=-2.469, p=0.014)、红细胞分布宽度(Z=-2.481, p=0.013)、平均血小板体积(Z=-2.668, p=0.008)均显著升高。血红蛋白(Z=-3.876, pZ=-3.005, p=0.003)、红细胞计数(F=0.248, pF=3.826, p=0.004)和红细胞压积(F=0.000, p>0.001)均显著降低。结论:结果提示MDD患者可能存在血清炎症反应,血液分析指标特别是平均血小板体积作为炎症的生物标志物具有潜在价值。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Relationship of Mean Platelet Volume To MDD: A Retrospective Study.
Background Results of numerous studies show that major depressive disorder (MDD) is associated with a chronic low-grade inflammation, but the underlying mechanism remains unclear. Aim To compare the results of blood cell analysis of MDD patients with healthy controls, and explore the potential value of it as an indicator of immune-inflammation in MDD, especially the mean platelet volume. Methods 103 MDD patients and 106 healthy controls with matched age and gender were recruited. We collected peripheral blood samples from both groups and gathered basic data. For comparison of normally distributed data (age, body mass index, lymphocyte count, white blood cell count, red blood cell count, hematocrit, platelet count and mean corpuscular volume) between groups, single t-test were used; and for comparison of non-normally distributed data (Neutrophil count, neutrophil count, platelet/ lymphocyte ratio, hemoglobin, red blood cell distribution width, mean platelet volume, mean hemoglobin concentration, mean hemoglobin and platelet distribution width), we used Mann-Whitney U-test. Results Compared with healthy controls, the MDD groups showed significantly higher white blood cell count (F=0.443, p=0.004), plateletcrit (F=8.3, p<0.001), neutrophil and lymphocyte ratio (Z=-6.063, p<0.001), neutrophil count (Z=-5.062, p<0.001), platelet/lymphocyte ratio (Z=-2.469, p=0.014), red blood cell distribution width (Z=-2.481, p=0.013) and mean platelet volume (Z=-2.668, p=0.008). In addition they had significantly lower hemoglobin (Z=-3.876, p<0.001), mean hemoglobin amount (Z=-3.005, p=0.003), red blood cell count (F=0.248, p<0.001), lymphocyte count (F=3.826, p=0.004) and hematocrit (F=0.000, p>0.001). Conclusions The results suggest that serum inflammatory response probably exists in people with MDD, and indicators of blood analysis especially mean platelet volume have a potential value as biomarker for inflammation.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
自引率
0.00%
发文量
2341
期刊介绍:
Shanghai archives of psychiatry (bimonthly) was founded in 1959 and is sponsored by Shanghai Mental Health Center. The journal is aimed at mental health workers across the country, including psychiatrists and nurses, clinical psychologists, social workers, and people who are committed to the cause of mental health. It focuses on reporting clinical research results and practical experience in the field of psychiatry, and introduces the latest knowledge in psychiatry and related fields. The columns include monographs, case reports, clinical case discussions, reviews, mental health and law, and debates and discussions.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


