脊柱性关节炎和非脊柱性关节炎患者骶髂关节磁共振成像病变的频率和解剖分布。
IF 3.4
2区 医学
Q2 RHEUMATOLOGY
Therapeutic Advances in Musculoskeletal Disease
Pub Date : 2022-09-05
eCollection Date: 2022-01-01
DOI:10.1177/1759720X221119245
引用次数: 1
摘要
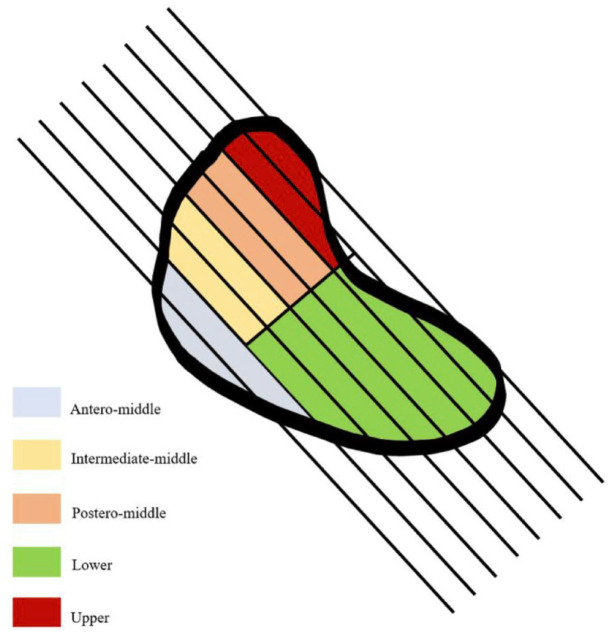
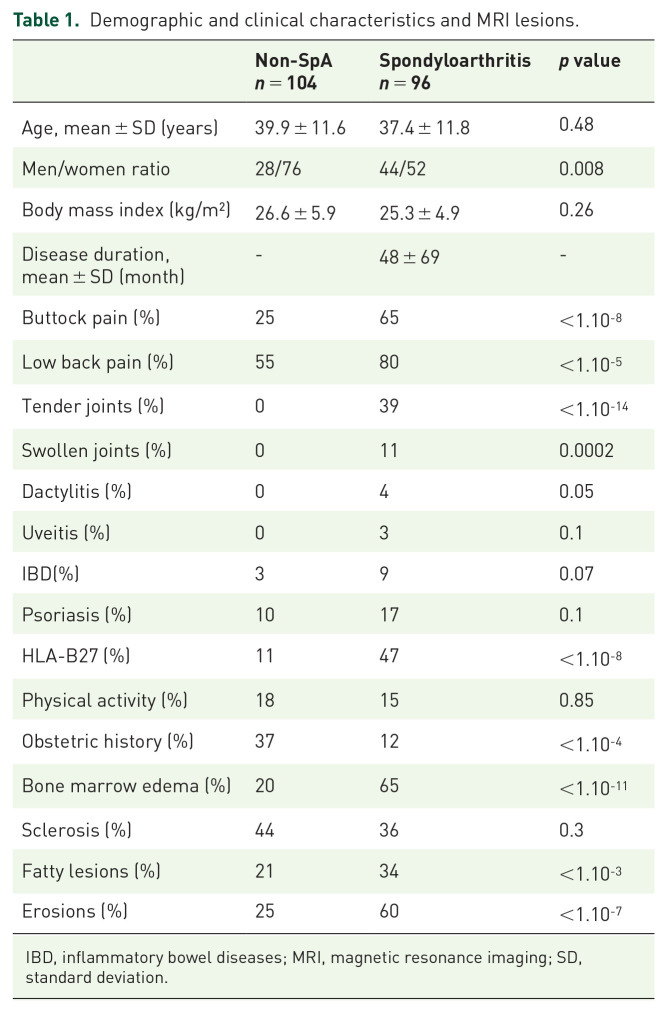
背景:骶髂关节的磁共振成像(MRI)对非影像学诊断轴性脊柱性关节炎至关重要。然而,在其他情况下可能会遇到炎症和结构性病变。目的:本研究的目的是评估和比较脊柱性关节炎(SpA)和非脊柱性关节炎(non-SpA)患者骶髂关节的mri炎症和结构性病变的频率和定位。设计:这是一项回顾性研究,包括200名患者,每位患者都接受了骶髂关节的MRI检查。方法:两位经验丰富的读者根据ASAS MRI工作组制定的定义对整套图像进行评估,以检测糜烂,软骨下硬化,脂肪病变,骨髓水肿(BME)和强直。我们将骶髂关节分为上、前-中、中-中、后-中、下五个节段。结果:共纳入96例SpA患者(平均年龄37.4±11.8岁)和104例非SpA患者(平均年龄39.9±11.6岁)。在96名SpA患者中,65%的患者有炎症性臀部疼痛,而非SpA组为25%。65%的SpA患者出现BME,主要发生在中-中段;20%的非SpA患者出现BME,主要发生在前-中段。44%的非SpA患者发生软骨下硬化,主要发生在前中段,而36%的SpA患者发生软骨下硬化。34%的SpA患者和21%的非SpA患者存在脂肪病变。25%的非SpA患者和60%的SpA患者出现糜烂。在非spa患者中,BME和结构性病变在后中段最小。结论:SpA组关节各节段均可见炎性及结构性病变,以中间节段为主,非SpA组病变以前-中间节段为主,后-中间节段少见。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Frequency and anatomic distribution of magnetic resonance imaging lesions in the sacroiliac joints of spondyloarthritis and non-spondyloarthritis patients.
Background: Lesions detected by magnetic resonance imaging (MRI) of the sacroiliac joints are critical to the diagnosis of non-radiographic axial spondyloarthritis. However, inflammatory and structural lesions may be encountered in other conditions. Objectives: The objective of this study was to evaluate and compare the frequency and localization of inflammatory and structural lesions on MRIs of the sacroiliac joint of spondyloarthritis (SpA) and non-spondyloarthritis (non-SpA) patients. Design: This is a retrospective study including 200 patients, each having undergone an MRI of the sacroiliac joints. Methods: Two experienced readers evaluated the whole set of images to detect erosions, subchondral sclerosis, fatty lesions, bone marrow edema (BME) and ankylosis according to the definitions established by the ASAS MRI working group. We divided sacroiliac joints into five segments: upper, antero-middle, intermediate-middle, postero-middle and lower. Results: A total of 96 subjects with SpA (mean age 37.4 ± 11.8 years) and 104 without SpA (mean age 39.9 ± 11.6 years) were included. Of the 96 SpA patients, 65% had inflammatory buttock pain compared with 25% in the non-SpA group. BME was seen in 65% of SpA patients, mainly in the intermediate-middle segment, and in 20% of non-SpA patients, predominantly in the antero-middle segment. Subchondral sclerosis occurred in 44% of non-SpA patients, mostly in the antero-middle segment, and in 36% of SpA patients. Fatty lesions were present in 34% of SpA and in 21% of non-SpA patients. Erosions were seen in 25% of non-SpA and in 60% of SpA patients. BME and structural lesions were minimally observed in the postero-middle segment in non-SpA patients. Conclusion: Inflammatory and structural lesions were observed in all segments of the joint in SpA, mainly in the middle segments, while lesions predominantly affected the antero-middle segment in non-SpA, and were uncommon in the postero-middle segment.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Therapeutic Advances in Musculoskeletal Disease
Medicine-Rheumatology
CiteScore
6.80
自引率
4.80%
发文量
132
审稿时长
18 weeks
期刊介绍:
Therapeutic Advances in Musculoskeletal Disease delivers the highest quality peer-reviewed articles, reviews, and scholarly comment on pioneering efforts and innovative studies across all areas of musculoskeletal disease.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


