Mirjam Tielen, Job van Exel, Mirjam Laging, Denise K Beck, Roshni Khemai, Teun van Gelder, Michiel G H Betjes, Willem Weimar, Emma K Massey
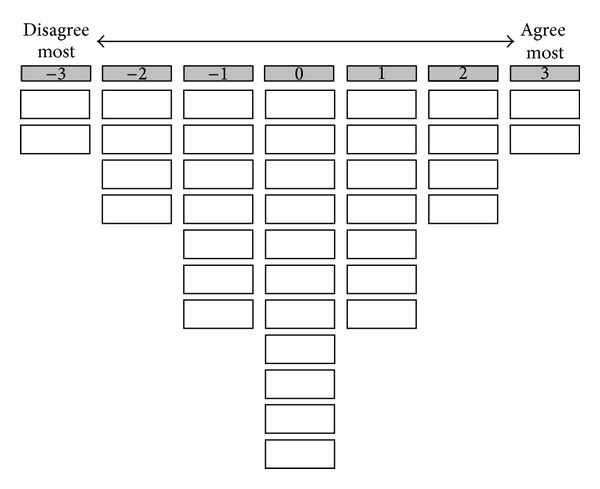
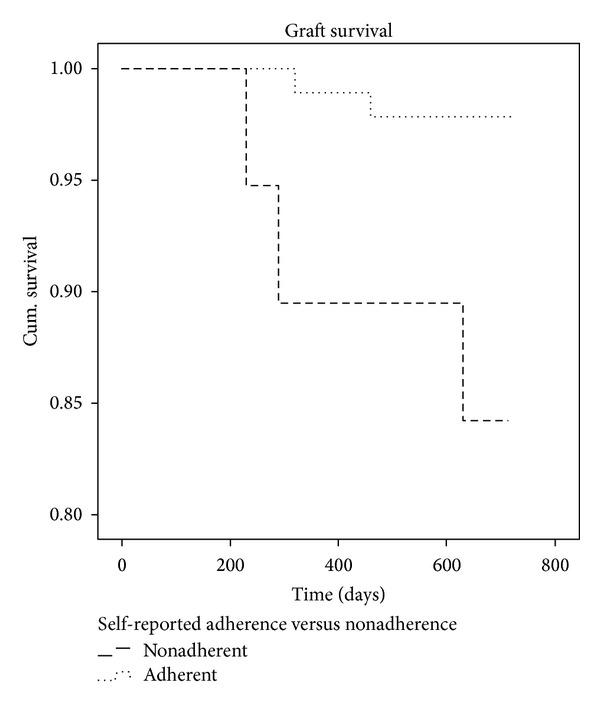
{"title":"肾移植术后用药态度及其与药物依从性和移植物存活的关系:一项2年随访研究。","authors":"Mirjam Tielen, Job van Exel, Mirjam Laging, Denise K Beck, Roshni Khemai, Teun van Gelder, Michiel G H Betjes, Willem Weimar, Emma K Massey","doi":"10.1155/2014/675301","DOIUrl":null,"url":null,"abstract":"<p><p>Background. Nonadherence to medication is a common problem after kidney transplantation. The aim of this study was to explore attitudes towards medication, adherence, and the relationship with clinical outcomes. Method. Kidney recipients participated in a Q-methodological study 6 weeks after transplantation. As a measure of medication adherence, respondents completed the Basel Assessment of Adherence to Immunosuppressive Medications Scale (BAASIS(©)-interview). Moreover, the intrapatient variability in the pharmacokinetics of tacrolimus was calculated, which measures stability of drug intake. Data on graft survival was retrieved from patient records up to 2 years after transplantation. Results. 113 renal transplant recipients (19-75 years old) participated in the study. Results revealed three attitudes towards medication adherence-attitude 1: \"confident and accurate,\" attitude 2: \"concerned and vigilant,\" and attitude 3: \"appearance oriented and assertive.\" We found association of attitudes with intrapatient variability in pharmacokinetics of tacrolimus, but not with self-reported nonadherence or graft survival. However, self-reported nonadherence immediately after transplantation was associated with lower two-year graft survival. Conclusion. These preliminary findings suggest that nonadherence shortly after kidney transplantation may be a risk factor for lower graft survival in the years to follow. The attitudes to medication were not a risk factor. </p>","PeriodicalId":45795,"journal":{"name":"Journal of Transplantation","volume":"2014 ","pages":"675301"},"PeriodicalIF":2.2000,"publicationDate":"2014-01-01","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://sci-hub-pdf.com/10.1155/2014/675301","citationCount":"72","resultStr":"{\"title\":\"Attitudes to medication after kidney transplantation and their association with medication adherence and graft survival: a 2-year follow-up study.\",\"authors\":\"Mirjam Tielen, Job van Exel, Mirjam Laging, Denise K Beck, Roshni Khemai, Teun van Gelder, Michiel G H Betjes, Willem Weimar, Emma K Massey\",\"doi\":\"10.1155/2014/675301\",\"DOIUrl\":null,\"url\":null,\"abstract\":\"<p><p>Background. Nonadherence to medication is a common problem after kidney transplantation. The aim of this study was to explore attitudes towards medication, adherence, and the relationship with clinical outcomes. Method. Kidney recipients participated in a Q-methodological study 6 weeks after transplantation. As a measure of medication adherence, respondents completed the Basel Assessment of Adherence to Immunosuppressive Medications Scale (BAASIS(©)-interview). Moreover, the intrapatient variability in the pharmacokinetics of tacrolimus was calculated, which measures stability of drug intake. Data on graft survival was retrieved from patient records up to 2 years after transplantation. Results. 113 renal transplant recipients (19-75 years old) participated in the study. Results revealed three attitudes towards medication adherence-attitude 1: \\\"confident and accurate,\\\" attitude 2: \\\"concerned and vigilant,\\\" and attitude 3: \\\"appearance oriented and assertive.\\\" We found association of attitudes with intrapatient variability in pharmacokinetics of tacrolimus, but not with self-reported nonadherence or graft survival. However, self-reported nonadherence immediately after transplantation was associated with lower two-year graft survival. Conclusion. These preliminary findings suggest that nonadherence shortly after kidney transplantation may be a risk factor for lower graft survival in the years to follow. The attitudes to medication were not a risk factor. </p>\",\"PeriodicalId\":45795,\"journal\":{\"name\":\"Journal of Transplantation\",\"volume\":\"2014 \",\"pages\":\"675301\"},\"PeriodicalIF\":2.2000,\"publicationDate\":\"2014-01-01\",\"publicationTypes\":\"Journal Article\",\"fieldsOfStudy\":null,\"isOpenAccess\":false,\"openAccessPdf\":\"https://sci-hub-pdf.com/10.1155/2014/675301\",\"citationCount\":\"72\",\"resultStr\":null,\"platform\":\"Semanticscholar\",\"paperid\":null,\"PeriodicalName\":\"Journal of Transplantation\",\"FirstCategoryId\":\"1085\",\"ListUrlMain\":\"https://doi.org/10.1155/2014/675301\",\"RegionNum\":0,\"RegionCategory\":null,\"ArticlePicture\":[],\"TitleCN\":null,\"AbstractTextCN\":null,\"PMCID\":null,\"EPubDate\":\"2014/4/28 0:00:00\",\"PubModel\":\"Epub\",\"JCR\":\"Q3\",\"JCRName\":\"SURGERY\",\"Score\":null,\"Total\":0}","platform":"Semanticscholar","paperid":null,"PeriodicalName":"Journal of Transplantation","FirstCategoryId":"1085","ListUrlMain":"https://doi.org/10.1155/2014/675301","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"2014/4/28 0:00:00","PubModel":"Epub","JCR":"Q3","JCRName":"SURGERY","Score":null,"Total":0}
引用次数: 72

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


