不同类型颈椎板成形术的疗效比较。
摘要
研究设计系统评价。研究的基本原理许多颈椎椎板成形术已经被描述过,但是很少有研究对这些技术进行比较,以确定它们之间的优越性。临床问题包括关键问题(KQ)1:对于后纵韧带骨化(OPLL)或颈椎病的成人颈椎病患者,开放式颈椎板成形术与法式门式颈椎板成形术的比较效果如何?KQ2:对于成年后骨髓型颈椎病或颈椎病患者,椎板成形术后使用微型钢板与不使用钢板的术后并发症(包括疼痛和感染)是否不同?KQ3:这些结果是否因术后早期宫颈活动而有所不同?材料和方法对1970年至2013年3月11日期间发表的英语文献进行系统综述。检索电子数据库和关键文献的参考文献列表,以确定评估(1)开放式颈椎板成形术和法式门颈椎板成形术的研究;(2)在颈椎板成形术中使用微型钢板或不使用钢板治疗成人脊髓型颈椎病或OPLL的研究。涉及创伤性发病、颈椎骨折、感染、畸形或肿瘤的研究被排除在外,非比较研究也被排除在外。两位独立审稿人(A.L.R, J.R.D.)使用推荐评估、发展和评价等级系统评估证据质量水平,分歧通过共识解决。结果我们确定了3项研究(1项证据等级[CoE] II和2项证据等级[CoE] III)符合我们的纳入标准,比较了开放式颈椎椎板成形术和法式椎板成形术,以及2项研究(1项证据等级为II和1项证据等级为III)比较了微型钢板和无钢板的使用。一项随机对照试验(RCT)和两项回顾性队列研究的数据表明,在脊髓病的改善方面,治疗组之间没有差异。一项随机对照试验报告了French door椎板成形术组轴向疼痛的显著改善和短形36评分的显著提高。总的来说,尽管所有研究中并发症的完整报告都很差,但开门组的并发症似乎比法式门组高。总的来说,一项随机对照试验和一项回顾性队列研究的数据表明,与微型钢板治疗组相比,无钢板治疗组的并发症(包括再手术、神经根病和感染)发生率更高。一项随机对照试验报告,无钢板治疗组的视觉模拟评分显示疼痛更大。尚无证据评估早期颈椎运动对开放式颈椎椎板成形术与法式门椎板成形术的影响。两项比较使用微型钢板和不使用钢板的研究均报道了术后早期运动。一项随机对照试验的证据表明,术后早期颈椎运动可能减轻疼痛。结论三个比较研究的数据不足以支持开门颈椎板成形术或法式门颈椎板成形术的优越性。两项比较研究的数据不足以支持颈椎板成形术后使用微型钢板或不使用钢板的优越性。支持任何结论的证据的总体强度很低或不足。因此,争论仍在继续,而脊柱外科社区有机会通过适当设计的临床研究来解决这些问题。

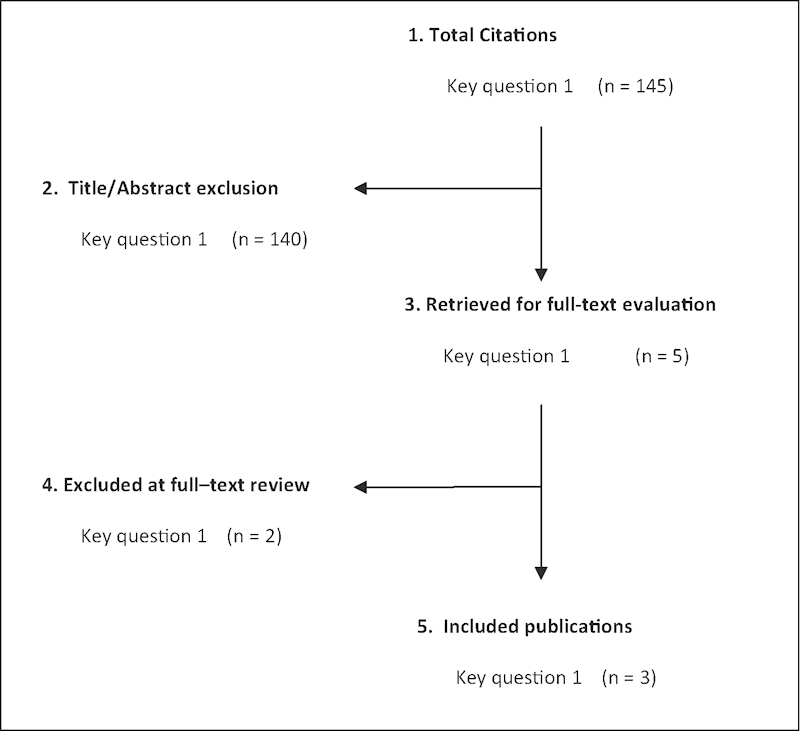

Study Design Systematic review. Study Rationale Numerous cervical laminoplasty techniques have been described but there are few studies that have compared these to determine the superiority of one over another. Clinical Questions The clinical questions include key question (KQ)1: In adults with cervical myelopathy from ossification of the posterior longitudinal ligament (OPLL) or spondylosis, what is the comparative effectiveness of open door cervical laminoplasty versus French door cervical laminoplasty? KQ2: In adults with cervical myelopathy from OPLL or spondylosis, are postoperative complications, including pain and infection, different for the use of miniplates versus the use of no plates following laminoplasty? KQ3: Do these results vary based on early active postoperative cervical motion? Materials and Methods A systematic review of the English-language literature was undertaken for articles published between 1970 and March 11, 2013. Electronic databases and reference lists of key articles were searched to identify studies evaluating (1) open door cervical laminoplasty and French door cervical laminoplasty and (2) the use of miniplates or no plates in cervical laminoplasty for the treatment of cervical spondylotic myelopathy or OPLL in adults. Studies involving traumatic onset, cervical fracture, infection, deformity, or neoplasms were excluded, as were noncomparative studies. Two independent reviewers (A.L.R., J.R.D.) assessed the level of evidence quality using the Grades of Recommendations Assessment, Development and Evaluation system, and disagreements were resolved by consensus. Results We identified three studies (one of class of evidence [CoE] II and two of CoE III) meeting our inclusion criteria comparing open door cervical laminoplasty with French door laminoplasty and two studies (one CoE II and one CoE III) comparing the use of miniplates with no plates. Data from one randomized controlled trial (RCT) and two retrospective cohort studies suggest no difference between treatment groups regarding improvement in myelopathy. One RCT reported significant improvement in axial pain and significantly higher short-form 36 scores in the French door laminoplasty treatment group. Overall, complications appear to be higher in the open door group than the French door group, although complete reporting of complications was poor in all studies. Overall, data from one RCT and one retrospective cohort study suggest that the incidence of complications (including reoperation, radiculopathy, and infection) is higher in the no plate treatment group compared with the miniplate group. One RCT reported greater pain as measured by the visual analog scale score in the no plate treatment group. There was no evidence available to assess the effect of early cervical motion for open door cervical laminoplasty compared with French door laminoplasty. Both studies comparing the use of miniplates and no plates reported early postoperative motion. Evidence from one RCT suggests that earlier postoperative cervical motion might reduce pain. Conclusion Data from three comparative studies are not sufficient to support the superiority of open door cervical laminoplasty or French door cervical laminoplasty. Data from two comparative studies are not sufficient to support the superiority of the use of miniplates or no plates following cervical laminoplasty. The overall strength of evidence to support any conclusions is low or insufficient. Thus, the debate continues while opportunity exists for the spine surgery community to resolve these issues with appropriately designed clinical studies.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


