自身免疫性肝炎中的自身抗体和自身抗原:临床实践和研究疾病发病机制的重要工具。
摘要
自身免疫性肝炎(AIH)是一种慢性肝脏坏死性炎症疾病,其特征是高丙种球蛋白血症、特征性自身抗体、与 HLA DR3 或 DR4 相关以及对免疫抑制治疗的良好反应。病因不明。在没有病毒、代谢、遗传和中毒性慢性肝炎或肝损伤病因的情况下,检测非器官和肝脏相关的自身抗体仍然是诊断该病的标志。本文报告了 AIH 目前的分类以及在该疾病中发现的几种自身抗体/目标自身抗原。此外,还阐述了这些标记物在鉴别诊断和 AIH 发病机制研究中的重要性。AIH 可细分为两大类型:AIH 1 型(AIH-1)和 AIH 2 型(AIH-2)。AIH-1 型的特征是检测到平滑肌自身抗体(SMA)和/或抗核抗体(ANA)。检测抗中性粒细胞胞浆自身抗体(ANCA)、抗淀粉样糖蛋白受体抗体(抗ASGP-R)和抗可溶性肝抗原或肝胰腺抗体(抗SLA/LP)可能有助于鉴别ANA/SMA血清阴性的患者。AIH-2的特点是存在针对肝脏和肾脏微粒体抗原的特异性自身抗体(抗LKM-1型或不常见的抗LKM-3型)和/或针对肝脏胞浆1抗原的自身抗体(抗LC1)。在一些慢性丙型肝炎(HCV)和慢性丁型肝炎(HDV)患者中也能检测到抗 LKM-1 和抗 LKM-3 自身抗体。细胞色素 P450 2D6 (CYP2D6) 已被证实是 AIH-2 和 HCV 感染中抗 LKM-1 自身抗体的主要靶抗原。最近有令人信服的数据表明,CYP2D6 在肝细胞表面的表达表明,抗 LKM-1 自身抗体在肝损伤中起着致病作用。UDP-糖醛酸转移酶家族 1 已被确定为抗 LKM-3 的靶自身抗原。因此,区分 AIH 和慢性病毒性肝炎(尤其是 HCV)尤为重要。最近,抗SLA/LP和抗LC1自身抗体的分子靶点被确定为一种50 kDa的UGA抑制tRNA相关蛋白和一种肝脏特异性酶--甲氨蝶呤环化酶。抗ASGP-R和抗LC1自身抗体似乎与疾病的严重程度和对治疗的反应密切相关,这表明这些自身抗体对肝细胞损伤具有致病作用。但一般来说,自身抗体不应被用于监测治疗、预测 AIH 的活动性或预后。最后,本文还介绍了一种特殊形式的 AIH,即自身免疫性多内分泌病-念珠菌病-外胚层营养不良综合征(APECED),它可能发生在一些患有罕见遗传综合征的患者身上。肝微粒体自身抗体(抗-LM)是在作为 APECED 疾病组成部分的 AIH 中检测到的特异性自身抗体,也可在二氢嗪诱发的肝炎病例中检测到。在与 APECED 相关的 AIH 和二氢嗪诱导的肝炎中,细胞色素 P450 1A2 被确定为抗 LM 自身抗体的靶自身抗原。后者可能表明,类似的自身免疫致病机制可导致易感个体的肝损伤,而与原发性缺陷无关。自身抗原-自身抗体复合物的特征描述仍然是一种极具吸引力的重要工具,可用于获得正确的诊断,并深入了解肝脏耐受性是如何被放弃以及 AIH 是如何产生的这一尚未解开的谜团。
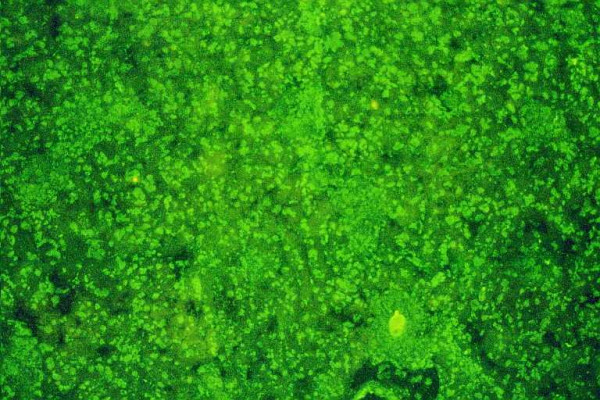
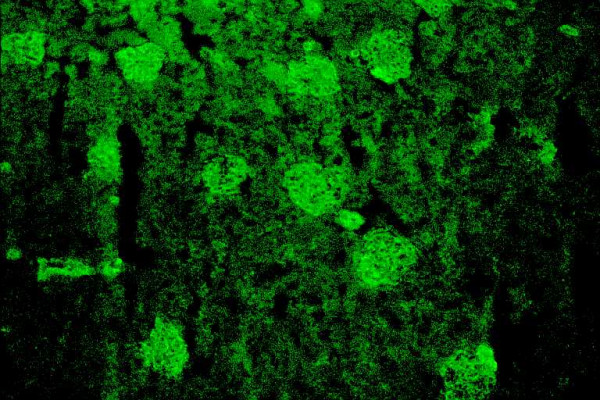
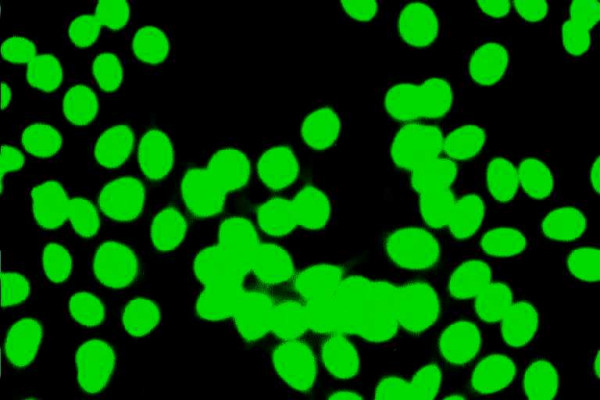
Autoimmune hepatitis (AIH) is a chronic necroinflammatory disease of the liver characterized by hypergammaglobulinemia, characteristic autoantibodies, association with HLA DR3 or DR4 and a favorable response to immunosuppressive treatment. The etiology is unknown. The detection of non-organ and liver-related autoantibodies remains the hallmark for the diagnosis of the disease in the absence of viral, metabolic, genetic, and toxic etiology of chronic hepatitis or hepatic injury. The current classification of AIH and the several autoantibodies/target-autoantigens found in this disease are reported. Current aspects on the significance of these markers in the differential diagnosis and the study of pathogenesis of AIH are also stated. AIH is subdivided into two major types; AIH type 1 (AIH-1) and type 2 (AIH-2). AIH-1 is characterized by the detection of smooth muscle autoantibodies (SMA) and/or antinuclear antibodies (ANA). Determination of antineutrophil cytoplasmic autoantibodies (ANCA), antibodies against the asialoglycoprotein receptor (anti-ASGP-R) and antibodies against to soluble liver antigens or liver-pancreas (anti-SLA/LP) may be useful for the identification of patients who are seronegative for ANA/SMA. AIH-2 is characterized by the presence of specific autoantibodies against liver and kidney microsomal antigens (anti-LKM type 1 or infrequently anti-LKM type 3) and/or autoantibodies against liver cytosol 1 antigen (anti-LC1). Anti-LKM-1 and anti-LKM-3 autoantibodies are also detected in some patients with chronic hepatitis C (HCV) and chronic hepatitis D (HDV). Cytochrome P450 2D6 (CYP2D6) has been documented as the major target-autoantigen of anti-LKM-1 autoantibodies in both AIH-2 and HCV infection. Recent convincing data demonstrated the expression of CYP2D6 on the surface of hepatocytes suggesting a pathogenetic role of anti-LKM-1 autoantibodies for the liver damage. Family 1 of UDP-glycuronosyltransferases has been identified as the target-autoantigen of anti-LKM-3. For these reasons the distinction between AIH and chronic viral hepatitis (especially of HCV) is of particular importance. Recently, the molecular target of anti-SLA/LP and anti-LC1 autoantibodies were identified as a 50 kDa UGA-suppressor tRNA-associated protein and a liver specific enzyme, the formiminotransferase cyclodeaminase, respectively. Anti-ASGP-R and anti-LC1 autoantibodies appear to correlate closely with disease severity and response to treatment suggesting a pathogenetic role of these autoantibodies for the hepatocellular injury. In general however, autoantibodies should not be used to monitor treatment, predict AIH activity or outcome. Finally, the current aspects on a specific form of AIH that may develop in some patients with a rare genetic syndrome, the autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy syndrome (APECED) are also given. Autoantibodies against liver microsomes (anti-LM) are the specific autoantibodies detected in AIH as a disease component of APECED but also in cases of dihydralazine-induced hepatitis. Cytochrome P450 1A2 has been identified as the target-autoantigen of anti-LM autoantibodies in both APECED-related AIH and dihydralazine-induced hepatitis. The latter may indicate that similar autoimmune pathogenetic mechanisms can lead to liver injury in susceptible individuals irrespective of the primary defect. Characterization of the autoantigen-autoantibody repertoire continues to be an attractive and important tool to get access to the correct diagnosis and to gain insight into the as yet unresolved mystery of how hepatic tolerance is given up and AIH ensues.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


