基于后踝相关韧带和踝关节稳定性的后踝骨折的分类和病理解剖
IF 5.9
1区 医学
Q1 ORTHOPEDICS
引用次数: 0
摘要
背景以往的后踝骨折分类主要基于骨折形态,临床意义有限。根据后踝相关韧带及踝关节稳定性、损伤机制及骨折形态,提出一种新的后踝骨折分类体系,以明确后踝骨折的病理解剖,指导临床诊治。方法采集20例新鲜冷冻下肢尸体标本,解剖后踝相关韧带,测量其胫骨止点范围、平均长度和方向。临床上,我们回顾性分析296例后踝骨折患者的影像学资料。将新鲜冷冻尸体标本后踝相关韧带的解剖测量与临床患者后踝骨折的CT成像资料相结合,建立了临床上实用的后踝骨折分类体系。并与Haraguci分类法和Mason分类法进行了比较。结果内踝后韧带包括胫骨后外侧至胫骨后内侧的胫腓后下韧带、胫腓下横韧带和胫腓后韧带。将296例后踝骨折分为三种类型。I型后踝骨折仅累及下胫腓横韧带胫骨止点(36例,12.2%)。Ⅱ型后踝骨折累及下胫腓横韧带和下胫腓后韧带的胫骨止点,根据是否存在关节软骨或模冲损伤分为2个亚型(ⅡA, 150例,50.7%;ⅡB, 79例,26.7%)。Ⅲ型后踝骨折累及胫骨下横腓骨、胫后下腓骨、胫后韧带的所有胫骨止点,根据后踝骨折碎片数分为2个亚型(ⅢA, 11例,3.7%;ⅢB, 20例,6.8%)。结论内踝骨折的形成是外力和内部韧带结构共同作用的结果。将后踝相关韧带与后踝骨折的分型相关联具有重要意义。该分类系统考虑了后踝相关韧带、损伤机制和骨折形态,从而明确了后踝骨折的病理解剖,对临床诊断和治疗具有指导意义。以往的后踝骨折分类主要基于骨折形态,临床意义有限。基于后踝相关韧带和踝关节稳定性、损伤机制和骨折形态,本研究提出了一种新的后踝骨折分类系统。该分类有助于更好地阐明后踝骨折的病理解剖,指导临床诊断和治疗。本文章由计算机程序翻译,如有差异,请以英文原文为准。
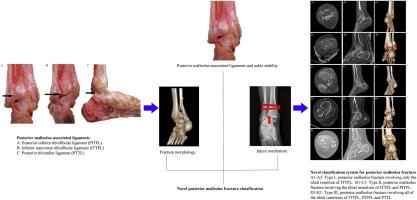
Classification and pathoanatomy of posterior malleolus fracture based on posterior malleolus-associated ligaments and ankle stability
Background
The clinical significance of previous posterior malleolus fracture classifications is limited because they are mainly based on fracture morphology. On the basis of posterior malleolus-associated ligaments and ankle stability, injury mechanism, and fracture morphology, a novel posterior malleolus fracture classification system was proposed to clarify the pathoanatomy of posterior malleolus fracture and guide clinical diagnosis and treatment.
Methods
Twenty fresh frozen cadaver specimens of the lower limbs were collected, posterior malleolus-associated ligaments were dissected, and the range of their tibial insertion, average length, and direction were measured. Clinically,we retrospectively analyzed the imaging information of 296 patients with posterior malleolus fractures. Correlating the anatomical measurements of posterior malleolus-associated ligaments of fresh frozen cadaver specimens with the computed tomography(CT) imaging data of posterior malleolus fracture of clinical patients, a clinically practical classification system of posterior malleolus fracture was established. In addition, the novel classification was compared with Haraguci classification and Mason classification.
Results
Posterior malleolus-associated ligaments include the posterior inferior tibiofibular, inferior transverse tibiofibular, and posterior tibiotalar ligaments from the posterolateral to posteromedial tibia. A total of 296 posterior malleolus fractures were divided into three types. Type I posterior malleolus fracture involved only the tibial insertion of the inferior transverse tibiofibular ligament (36 cases, 12.2 %). Type Ⅱ posterior malleolus fracture involved the tibial insertions of the inferior transverse tibiofibular and posterior inferior tibiofibular ligaments and was divided into two subtypes according to whether or not articular cartilage or die-punch injury was present (ⅡA, 150 cases, 50.7 %; ⅡB, 79 cases, 26.7 %). Type Ⅲ posterior malleolus fracture involved all the tibial insertions of the inferior transverse tibiofibular, posterior inferior tibiofibular, and posterior tibiotalar ligaments and included two subtypes according to the fragment number of posterior malleolus fracture (ⅢA, 11 cases, 3.7 %; ⅢB, 20 cases, 6.8 %).
Conclusions
The formation of posterior malleolus fracture stems from the combined effects of external force and internal ligament structure. Correlating posterior malleolus-associated ligaments with the classification of posterior malleolus fracture is of great significance. The proposed classification system considers posterior malleolus-associated ligaments, injury mechanism, and fracture morphology and thus clarifies the pathoanatomy of posterior malleolus fracture and serves as a guide for clinical diagnosis and treatment.
The translational potential of this article
The clinical significance of previous posterior malleolus fracture classifications is limited because they are mainly based on fracture morphology. On the basis of posterior malleolus-associated ligaments and ankle stability, injury mechanism, and fracture morphology, a novel posterior malleolus fracture classification system in our study was proposed. The classification promoted better elucidation of the pathoanatomy of posterior malleolus fracture and guidance for clinical diagnosis and treatment.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Journal of Orthopaedic Translation
Medicine-Orthopedics and Sports Medicine
CiteScore
11.80
自引率
13.60%
发文量
91
审稿时长
29 days
期刊介绍:
The Journal of Orthopaedic Translation (JOT) is the official peer-reviewed, open access journal of the Chinese Speaking Orthopaedic Society (CSOS) and the International Chinese Musculoskeletal Research Society (ICMRS). It is published quarterly, in January, April, July and October, by Elsevier.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


