舌下神经移植与舌下跳神经移植用于面部恢复的比较:系统综述
IF 2.4
3区 医学
Q2 SURGERY
Journal of Plastic Reconstructive and Aesthetic Surgery
Pub Date : 2025-08-29
DOI:10.1016/j.bjps.2025.08.029
引用次数: 0
摘要
面瘫通过损害面部表情、语言和吞咽显著影响患者的生活质量。舌下神经移植(HNT)和舌下跳神经移植(HJG)是一种成熟的面部再生手术技术,各有其独特的优势和并发症。本系统综述比较了HNT和HJG的功能结局和并发症,以指导最佳手术决策。方法按照系统评价和荟萃分析指南的首选报告项目,对7个数据库进行系统评价。比较HNT(端到端[ETE]或端到端[ETS])和HJG技术在成人面瘫中的应用。主要结果包括通过House-Brackmann (HB)量表、Sunnybrook评分系统、FaCE调查或面部残疾指数评估的面部运动恢复。次要结局包括并发症发生率、生活质量和手术成功的预测因素。使用rob2、Newcastle-Ottawa量表和ROBINS-I工具评估偏倚风险。结果共纳入34项研究,1008例患者。HNT (ETE)提供了强有力的面部恢复,但与高舌头萎缩率(73%)和语言/吞咽困难(57%)相关。HNT (ETS)保留了部分舌下功能,降低了发病率,同时保持了良好的结果(HB II-III恢复率为78-86%)。HJG最大限度地减少了并发症,62.5-91.6%的患者无严重舌萎缩和HB II-III恢复。由于神经移植而接受HJG的患者恢复较慢,但长期改善了面部对称性和减少了联动性。结论HNT和HJG对面部再生均有较好的疗效。HNT (ETE)恢复更快,但发病率更高,而HJG最大限度地减少并发症并保持功能预后。HNT (ETS)提供了疗效和发病率之间的平衡。未来的比较研究需要使用标准化的结果测量,以积累的临床经验和已发表的结果为指导,完善针对患者的手术选择。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Comparison of hypoglossal nerve transfer and hypoglossal jump nerve graft techniques for facial reanimation: A systematic review
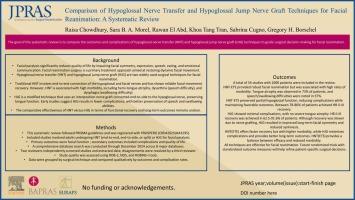
Background
Facial paralysis significantly affects patient quality of life by impairing facial expression, speech, and swallowing. Hypoglossal nerve transfer (HNT) and hypoglossal jump nerve graft (HJG) are established surgical techniques for facial reanimation, each with distinct advantages and complications. This systematic review compares the functional outcomes and complications of HNT and HJG to guide optimal surgical decision making.
Methods
Following Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, a systematic review was conducted across 7 databases. Studies comparing HNT (end-to-end [ETE] or end-to-side [ETS]) and HJG techniques in adults with facial paralysis were included. Primary outcomes included facial movement recovery assessed via the House-Brackmann (HB) scale, Sunnybrook grading system, FaCE survey, or Facial Disability Index. Secondary outcomes included complication rates, quality of life, and predictors of surgical success. Risk of bias was assessed using ROB-2, Newcastle-Ottawa Scale, and ROBINS-I tools.
Results
A total of 34 studies comprising 1008 patients were included. HNT (ETE) provided robust facial reanimation but was associated with high rates of tongue atrophy (73%) and speech/swallowing difficulties (57%). HNT (ETS) preserved partial hypoglossal function and reduced morbidity while maintaining favorable outcomes (HB II–III recovery in 78–86%). HJG minimized complications, with no severe tongue atrophy and HB II–III recovery in 62.5–91.6% of patients. Recovery was slower in patients who underwent HJG due to nerve grafting but resulted in improved long-term facial symmetry and reduced synkinesis.
Conclusion
Both HNT and HJG are effective for facial reanimation. HNT (ETE) offers faster recovery but has higher morbidity, while HJG minimizes complications and maintains functional outcomes. HNT (ETS) provides a balance between efficacy and morbidity. Future comparative studies using standardized outcome measures are needed to refine patient-specific surgical selection, guided by accumulated clinical experience and published outcomes.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
3.10
自引率
11.10%
发文量
578
审稿时长
3.5 months
期刊介绍:
JPRAS An International Journal of Surgical Reconstruction is one of the world''s leading international journals, covering all the reconstructive and aesthetic aspects of plastic surgery.
The journal presents the latest surgical procedures with audit and outcome studies of new and established techniques in plastic surgery including: cleft lip and palate and other heads and neck surgery, hand surgery, lower limb trauma, burns, skin cancer, breast surgery and aesthetic surgery.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


