tizepatide是GLP-1和GIP受体双激动剂,通过肠道微生物相关代谢物促进肥胖小鼠骨质流失
IF 5.9
1区 医学
Q1 ORTHOPEDICS
引用次数: 0
摘要
tizepatide (TZP)是一种新型的双糖依赖性胰岛素性多肽(GIP)和胰高血糖素样肽1 (GLP-1)受体激动剂,最近被批准用于治疗2型糖尿病(T2DM)和肥胖;然而,TZP在骨重塑中的作用尚不清楚。通过体外诱导骨髓间充质细胞(BMSCs)分化,观察替西帕肽对成骨细胞和破骨细胞的影响。2. 以Db/ Db小鼠为病理模型,研究TZP对骨代谢的影响。在TZP干预后,收集小鼠肠道粪便进行16s rRNA基因测序,选择与骨量最相关的候选肠道菌群,并通过随后的菌群补充实验验证肠道菌群对骨代谢的影响。3. 利用代谢组学方法分析了添加候选微生物群与未添加候选微生物群小鼠粪便代谢物的差异,并通过BMSCs诱导分化实验中差异代谢物的体外干预验证了候选代谢物对骨代谢的影响。结果我们发现,TZP干预导致体内骨量累积显著减少。TZP对体外成骨细胞和破骨细胞的分化并不是必不可少的。肠道菌群调节骨骼和脂肪的稳态。我们进一步证明,在TZP治疗后,db/db小鼠肠道微生物群的生物多样性发生了显著改变。肠道菌群中促成骨的关键成分毛螺科显著减少。作为毛缕菌科的主要代谢物,evolodiamine在体外具有抑制破骨细胞生成的作用。在此基础上,移植毛螺科植物可有效改善因TZP治疗而导致的db/db小鼠骨质流失。结论TZP可导致糖尿病和肥胖患者的骨质流失,针对TZP治疗的2型糖尿病患者的肠道菌群组成可能提供一种保护骨骼健康的潜在途径。本研究提示TZP对骨量有负面影响,提示临床应重视替西帕肽治疗后骨量进一步下降的风险,并有必要对其骨代谢进行随访。此外,肠道微生物群在骨代谢调节中起重要作用,补充某些益生菌可能对TZP治疗相关的骨量减少具有预防作用。我们的研究为今后T2DM患者药物相关性骨质疏松的防治提供参考。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Tirzepatide, a dual GLP-1 and GIP receptor agonist, promotes bone loss in obese mice via gut microbial-related metabolites
Background
As a novel dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide 1 (GLP-1) receptor agonist, Tirzepatide (TZP) is a recently approved medication for treating type 2 diabetes mellitus (T2DM) and obesity; however, the effect of TZP in bone remodeling remains unclear.
Methods
1. The effect of Tirzepatide on osteoblasts and osteoclasts was observed by inducing differentiation of bone marrow mesenchymal cells (BMSCs) in vitro. 2. Db/db mice were used as a pathological model to investigate the role of TZP on bone metabolism. After TZP intervention, the feces in the intestinal tract of mice were collected for 16s rRNA gene sequencing to select the candidate gut microbiota most related to bone mass, and the effects of gut microbiota on bone metabolism were verified through subsequent microbiota supplementation experiments. 3. Metabolomics was used to analyze the difference of fecal metabolites between mice with the candidate microbiota supplement and those without, and the effect of candidate metabolites on bone metabolism was verified by the in vitro intervention of differential metabolites in BMSCs induction differentiation experiments.
Results
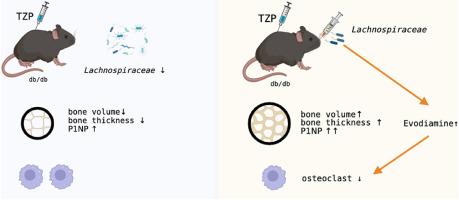
We found that TZP intervention resulted in a significant decrease in bone mass accrual in vivo. TZP was not indispensable to the differentiation of osteoblasts and osteoclasts in vitro. Bone and fat homeostasis were modulated by gut microbiota. We further demonstrated that the biodiversity of the gut microbiota in db/db mice was strikingly altered after TZP treatment. Lachnospiraceae, a key pro-osteogenic component of gut microbiota was significantly reduced. As a main metabolite of Lachnospiraceae, evodiamine played a role in suppressing osteoclastogenesis in vitro. Based on this, the transplantation of the Lachnospiraceae effectively ameliorated bone loss that was seen in db/db mice due to TZP treatment.
Conclusion
TZP administration leads to bone loss in the context of diabetes and obesity, and targeting the composition of gut microbiota may provide a potential way to protect bone health in type 2 diabetic patients treating with TZP.
The translational potential of this article
This study indicates that TZP has a negative impact on bone mass, suggesting that clinical attention should be paid to the risk of further decline in bone mass after Tirzepatide treatment, and it is necessary to follow up on their bone metabolism. Additionally, the gut microbiota plays an important role in bone metabolism regulation, and supplementing with certain probiotics may have a preventive effect on bone mass reduction associated with TZP treatment. Our research provides a reference for the prevention and treatment of drug-related osteoporosis in patients with T2DM in the future.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Journal of Orthopaedic Translation
Medicine-Orthopedics and Sports Medicine
CiteScore
11.80
自引率
13.60%
发文量
91
审稿时长
29 days
期刊介绍:
The Journal of Orthopaedic Translation (JOT) is the official peer-reviewed, open access journal of the Chinese Speaking Orthopaedic Society (CSOS) and the International Chinese Musculoskeletal Research Society (ICMRS). It is published quarterly, in January, April, July and October, by Elsevier.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


