心衰患者经导管主动脉瓣置换术的结果:来自国家再入院数据库的见解
IF 1.9
Q3 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
背景:射血分数对心衰(HF)患者经导管主动脉瓣置换术(TAVR)后预后的影响尚不清楚。方法使用国家再入院数据库(2016-2020),识别接受TAVR的成年HF患者,并比较射血分数降低(HFrEF)和射血分数保持(HFpEF)的结果。主要结局是全因住院患者死亡率,次要结局包括大出血、充血红细胞(pRBC)输注、急性肾损伤(AKI)、缺血性脑血管事故(CVA)、瓣膜并发症、转开腹手术、住院时间和总费用。结果在231,092例接受TAVR的HF患者中,89,782例有HFrEF。与HFpEF患者相比,HFrEF患者的住院死亡率较高(调整优势比[aOR] 1.97, 95% CI 1.78-2.19, P < 0.001)、大出血(aOR 1.49, 95% CI 1.36-1.63, P < 0.001)、pRBC输注(aOR 1.28, 95% CI 1.19-1.38, P < 0.001)、AKI (aOR 1.89, 95% CI 1.79-1.99, P < 0.001)、瓣膜并发症(aOR 1.41, 95% CI 1.21-1.64, P < 0.001)、转行开放手术(aOR 1.72, 95% CI 1.28 - 2.34, P < 0.001)。缺血性CVA无显著差异(aOR 1.12, 95% CI 0.97-1.29, P = 0.13)。HFrEF还与较长的住院时间(调整平均差[aMD] 2.06天,95% CI 1.93-2.18, P < 0.001)和较高的总费用(aMD 29,783美元,95% CI 25,106-34,460美元,P < 0.001)相关。结论与HFpEF患者相比,HFrEF患者接受TAVR的预后更差。这些发现强调了在对心衰患者进行TAVR手术前进行细致的患者选择和风险评估的必要性。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Outcomes of transcatheter aortic valve replacement in heart failure patients: Insights from the National Readmission Database
Background
The effect of ejection fraction on outcomes after transcatheter aortic valve replacement (TAVR) in heart failure (HF) patients remains unclear.
Methods
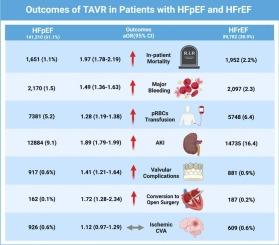
Using the National Readmission Database (2016–2020), adult HF patients who underwent TAVR were identified, and outcomes were compared between those with reduced ejection fraction (HFrEF) and preserved ejection fraction (HFpEF). The primary outcome was all-cause inpatient mortality, while secondary outcomes included major bleeding, packed red blood cell (pRBC) transfusion, acute kidney injury (AKI), ischemic cerebrovascular accidents (CVA), valvular complications, conversion to open surgery, length of stay, and total charges.
Results
Among 231,092 HF patients who underwent TAVR, 89,782 had HFrEF. Compared to HFpEF patients, HFrEF was associated with higher inpatient mortality (adjusted odds ratio [aOR] 1.97, 95 % CI 1.78–2.19, P < 0.001), major bleeding (aOR 1.49, 95 % CI 1.36–1.63, P < 0.001), pRBC transfusion (aOR 1.28, 95 % CI 1.19–1.38, P < 0.001), AKI (aOR 1.89, 95 % CI 1.79–1.99, P < 0.001), valvular complications (aOR 1.41, 95 % CI 1.21–1.64, P < 0.001), and conversion to open surgery (aOR 1.72, 95 % CI 1.28–2.34, P < 0.001), with no significant difference in ischemic CVA (aOR 1.12, 95 % CI 0.97–1.29, P = 0.13). HFrEF was also associated with longer hospital stays (adjusted mean difference [aMD] 2.06 days, 95 % CI 1.93–2.18, P < 0.001) and higher total charges (aMD $29,783, 95 % CI 25,106–34,460, P < 0.001).
Conclusion
Patients with HFrEF undergoing TAVR experienced worse outcomes compared to those with HFpEF. These findings underscore the need for meticulous patient selection and risk evaluation before performing TAVR in HF patients.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Cardiovascular Revascularization Medicine
CARDIAC & CARDIOVASCULAR SYSTEMS-
CiteScore
3.30
自引率
5.90%
发文量
687
审稿时长
36 days
期刊介绍:
Cardiovascular Revascularization Medicine (CRM) is an international and multidisciplinary journal that publishes original laboratory and clinical investigations related to revascularization therapies in cardiovascular medicine. Cardiovascular Revascularization Medicine publishes articles related to preclinical work and molecular interventions, including angiogenesis, cell therapy, pharmacological interventions, restenosis management, and prevention, including experiments conducted in human subjects, in laboratory animals, and in vitro. Specific areas of interest include percutaneous angioplasty in coronary and peripheral arteries, intervention in structural heart disease, cardiovascular surgery, etc.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


