基于深度学习的左侧淋巴结阴性乳腺癌放疗计划的多中心评价
IF 3.3
Q2 ONCOLOGY
引用次数: 0
摘要
背景与目的基于深度学习的放射治疗计划(DLP)具有提高放射治疗计划一致性和效率的潜力。然而,其临床适用性仍然有限,部分原因是需要将预测剂量转化为可交付剂量。本研究通过评估其性能和开发标准化翻译参数集,评估了跨多个机构的特定机构DLP解决方案的通用性。材料与方法4家机构对15例左侧淋巴结阴性乳腺癌患者提供临床治疗方案。使用基于某机构数据训练的深度学习预测模型生成提供40.05 Gy的治疗方案。通过将初始参数设置(InitialMimick)应用于来自其他三个机构的数据集(n = 45),使用国家共识标准进行外部验证。然后根据来自所有四家机构的数据(n = 12)开发标准化参数集(GenericMimick),然后对数据集中剩余的48名患者进行评估。结果initialmimick计划在Dmean (40.5 vs. 40.1 Gy)和D2% (42.4 vs. 41.4 Gy)的计划目标体积中显示更高的平均剂量值,与临床计划(25/45)相比,达到所有临床目标(15/45)的病例较少。经过参数调整后,GenericMimick计划导致更多的计划达到所有目标(28/48),与临床计划(30/48)相当,Dmean为40.3 vs. 40.1 Gy, D2%为41.9 vs. 41.5 Gy。有危险器官的平均差异平均剂量小于0.2戈瑞。结论具有标准化翻译参数集的dlp在多个机构中具有普遍适用性。本文章由计算机程序翻译,如有差异,请以英文原文为准。
A multi-centre evaluation of deep learning based radiotherapy planning for left-sided node-negative breast cancer
Background and Purpose
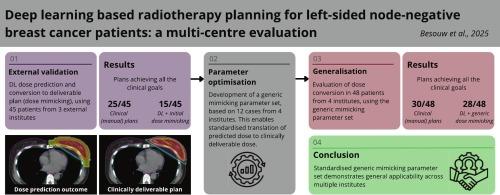
Deep learning based planning (DLP) has the potential to improve consistency and efficiency in radiotherapy treatment planning. However, its clinical applicability remains limited, partly due to the need to translate a predicted dose into a deliverable dose. This study evaluated the generalisability of an institution specific DLP solution across multiple institutions by assessing its performance and developing a standardised translation parameter set.
Materials and Methods
Four institutions provided clinical treatment plans of 15 patients with left-sided node-negative breast cancer. Treatment plans delivering 40.05 Gy were generated using a deep learning prediction model trained on data from one institution. External validation was performed using national consensus criteria, by applying the initial parameter settings (InitialMimick) to datasets (n = 45) from three other institutions. A standardised parameter set (GenericMimick) was then developed based on data (n = 12) from all four institutions, whereafter it was evaluated on the remaining 48 patients of the dataset.
Results
InitialMimick plans showed higher average dose values in the planning target volume for the Dmean (40.5 vs. 40.1 Gy) and D2% (42.4 vs. 41.4 Gy), with fewer cases meeting all clinical goals (15/45) compared to clinical plans (25/45). After parameter adjustment, GenericMimick plans resulted in more plans meeting all goals (28/48), comparable to the clinical plans (30/48), with Dmean of 40.3 vs. 40.1 Gy and D2% of 41.9 vs. 41.5 Gy. Mean differences in organs at risk mean doses were less than 0.2 Gy.
Conclusion
DLP with a standardised translation parameter set demonstrated general applicability across multiple institutions.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Physics and Imaging in Radiation Oncology
Physics and Astronomy-Radiation
CiteScore
5.30
自引率
18.90%
发文量
93
审稿时长
6 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


