免疫性血小板减少症患者血栓形成风险的地理和诊断差异:一项系统回顾和荟萃分析
IF 3.4
3区 医学
Q1 HEMATOLOGY
引用次数: 0
摘要
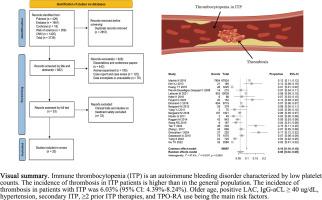
背景:虽然免疫性血小板减少症(ITP)主要以出血表现为特征,但新出现的证据表明对血栓事件有矛盾的倾向。本研究旨在系统评价ITP患者血栓形成的发生率,识别相关危险因素,为临床实践提供循证指导。方法检索spubmed、EMBASE、Cochrane Library、Web of Science和中国知网(CNKI)自各数据库建立至2025年4月1日有关ITP患者血栓形成的文献。两名独立研究人员使用纽卡斯尔-渥太华量表(NOS)进行研究选择、数据提取和质量评估。采用R软件进行统计分析。结果从20项纳入的研究中,包括100,446例ITP患者,我们确定了9010例血栓形成事件。合并血栓发生率为6.03 %(95 % CI: 4.39-8.24),在校正发表偏倚后增加至10.43 %(95 % CI: 7.17-14.93)。观察到显著的区域差异(北美:7.13 %;亚洲:4.50 %;欧洲:6.92 %)。发病率也因诊断标准而异,从2.08 % (2020 CMACSH)到8.18 % (2011 ASH)不等。没有发现基于性别或血栓类型的显著差异。重要独立危险因素包括高龄(HR = 7.53),狼疮抗凝积极性(HR = 9.9),高架IgG-aCL (HR = 7.5)、高血压(HR = 4.12),多个疗法(HR = 3.19)之前,二级ITP (HR = 1.29),和使用促血小板生成素受体受体激动剂(HR = 3.15)。结论ITP患者血栓形成风险明显增加,高危人群需要有针对性的筛查和预防策略。未来的研究应侧重于高质量、多中心的前瞻性队列研究,并开发更准确的血栓形成风险预测模型,以指导临床决策。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Geographic and diagnostic variations in thrombosis risk among patients with immune thrombocytopenia: A systematic review and meta-analysis
Background
While immune thrombocytopenia (ITP) is primarily characterized by bleeding manifestations, emerging evidence suggests a paradoxical predisposition to thrombotic events. This study aims to systematically evaluate the incidence of thrombosis in patients with ITP and identify associated risk factors, thereby providing evidence-based guidance for clinical practice.
Methods
PubMed, EMBASE, Cochrane Library, Web of Science, and CNKI were searched for literature on thrombosis in ITP patients from the inception of each database to April 1, 2025. Two independent researchers conducted study selection, data extraction, and quality assessment using the Newcastle-Ottawa Scale (NOS). Statistical analyses were performed using R software.
Results
From 20 included studies involving 100,446 ITP patients, we identified 9010 thrombotic events. The pooled incidence of thrombosis was 6.03 % (95 % CI: 4.39–8.24), increasing to 10.43 % (95 % CI: 7.17–14.93) after trim-and-fill adjustment for publication bias. Significant regional variation was observed (North America: 7.13 %; Asia: 4.50 %; Europe: 6.92 %). Incidence also varied by diagnostic criteria, ranging from 2.08 % (2020 CMACSH) to 8.18 % (2011 ASH). No significant differences were found based on gender or type of thrombosis. Key independent risk factors included advanced age (HR = 7.53), lupus anticoagulant positivity (HR = 9.9), elevated IgG-aCL (HR = 7.5), hypertension (HR = 4.12), multiple prior therapies (HR = 3.19), secondary ITP (HR = 1.29), and the use of thrombopoietin receptor agonists (HR = 3.15).
Conclusion
Patients with ITP have a significantly increased risk of thrombosis, highlighting the need for targeted screening and preventive strategies in high-risk populations. Future research should focus on high-quality, multicenter prospective cohort studies and the development of more accurate thrombotic risk prediction models to guide clinical decision-making.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Thrombosis research
医学-外周血管病
CiteScore
14.60
自引率
4.00%
发文量
364
审稿时长
31 days
期刊介绍:
Thrombosis Research is an international journal dedicated to the swift dissemination of new information on thrombosis, hemostasis, and vascular biology, aimed at advancing both science and clinical care. The journal publishes peer-reviewed original research, reviews, editorials, opinions, and critiques, covering both basic and clinical studies. Priority is given to research that promises novel approaches in the diagnosis, therapy, prognosis, and prevention of thrombotic and hemorrhagic diseases.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


