西马鲁肽2.4 mg对美国心力衰竭患者医疗资源利用和医疗费用的影响(SHINE-HF)。
IF 3.6
4区 医学
Q2 PHARMACOLOGY & PHARMACY
引用次数: 0
摘要
目的:肥胖是心衰(HF)早期发展的危险因素,心衰是最昂贵的肥胖相关疾病之一。临床试验已经证明,2.4 mg西马鲁肽可改善心衰患者的预后。该研究的目的是比较接受2.4 mg西马鲁肽治疗和未接受治疗的超重或肥胖和心衰患者的总全因医疗费用和医疗资源利用率(HCRU)。方法:本研究采用Komodo医疗地图©进行回顾性、非介入性队列研究,纳入基线期住院或门诊HF索赔≥1例、超重或肥胖、在索引日期前后连续接受医疗和药房登记≥12个月的患者。如果患者在2021年6月4日至2023年9月30日期间首次服用西马鲁肽2.4 mg,则被纳入治疗组。随机选择未使用semaglutide的对照组,并根据基线人口统计学、临床特征、医疗费用和HCRU将倾向评分与接受治疗的患者相匹配。采用准泊松分布的广义线性模型比较医疗费用和HCRU率。研究结果:在开始使用semaglutide 2.4 mg治疗后的一年中,与未使用semaglutide 2.4 mg治疗的患者相比,平均全因医疗费用降低了28%(- 8,544美元)(19,094美元vs 27,638美元/患者/年[PPPY];调整成本比[aCR] = 0.72, 95%可信区间[CI] 0.60-0.84];P < 0.001)。semaglutide 2.4 mg的住院费用比对照组低55%(- 6304美元)(4,377美元对10,681美元;aCR = 0.45 [95% CI 0.26-0.64];P < 0.001),治疗组住院就诊率PPPY比对照组低42% (0.15 vs. 0.26;调整后住院就诊率比值= 0.58 [95% CI 0.38-0.78];P < 0.001)。西马鲁肽2.4 mg组的平均门诊接诊率更高(36.6比31.6;P = 0.027),但门诊费用略低(13,366美元对15,654美元;aCR = 0.88;95% ci 0.74-1.03;P = 0.11),使用semaglutide 2.4 mg,表明门诊次数较多,但强度较低。在急诊费用或就诊率方面没有发现差异。意义:对美国大型行政索赔数据库的现实世界分析显示,与未接受塞马鲁肽2.4 mg治疗的超重或肥胖和HF患者相比,接受塞马鲁肽2.4 mg治疗的患者的医疗费用和住院资源利用率显著降低。在这些患者中使用2.4 mg的西马鲁肽改善预后,同时降低成本和HCRU,有助于控制美国日益增长的心衰负担。本文章由计算机程序翻译,如有差异,请以英文原文为准。
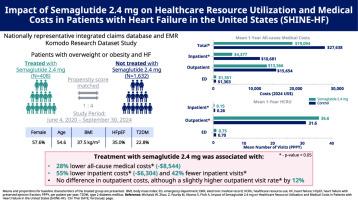
Impact of Semaglutide 2.4 mg on Healthcare Resource Utilization and Medical Costs in Patients With Heart Failure in the United States (SHINE-HF)
Purpose
Obesity is a risk factor for premature development of heart failure (HF), one of the costliest obesity-related disorders. Clinical trials have demonstrated the efficacy of semaglutide 2.4 mg in improving outcomes in patients with HF. The study objective is to compare total all-cause medical costs and healthcare resource utilization (HCRU) among patients with overweight or obesity and HF treated with semaglutide 2.4 mg versus those not treated.
Methods
This retrospective, noninterventional, cohort study using the Komodo Healthcare Map© included patients with ≥1 inpatient or outpatient claim for HF during the baseline period, with overweight or obesity, and ≥12 months of continuous medical and pharmacy enrollment prior to and after the index date. Patients were included in the treated group if they first filled a prescription for semaglutide 2.4 mg between June 4, 2021-September 30, 2023. Semaglutide-untreated controls were randomly selected and propensity score matched to treated patients based on baseline demographics, clinical characteristics, medical costs, and HCRU. Medical costs and HCRU rates were compared using generalized linear models with a quasi-Poisson distribution.
Findings
In the year following treatment initiation with semaglutide 2.4 mg, mean all-cause medical costs were 28% lower (–$8,544) compared with patients not treated with semaglutide 2.4 mg ($19,094 vs $27,638 per patient per year [PPPY]; adjusted cost ratio [aCR] = 0.72, 95% confidence interval [CI] 0.60–0.84]; P < 0.001). Inpatient costs with semaglutide 2.4 mg were 55% lower (–$6,304) than controls ($4,377 vs $10,681; aCR = 0.45 [95% CI 0.26–0.64]; P < 0.001) and the inpatient visit rate PPPY was 42% lower in treated patients versus controls (0.15 vs. 0.26; adjusted inpatient visit rate ratio = 0.58 [95% CI 0.38–0.78]; P < 0.001). The mean outpatient visit rate was higher in the semaglutide 2.4 mg-treated group (36.6 vs. 31.6; P = 0.027), but outpatient costs were slightly lower ($13,366 vs. $15,654; aCR = 0.88; 95% CI 0.74–1.03; P = 0.11) with semaglutide 2.4 mg, indicating more frequent outpatient services, but at a lower intensity level. No difference was found in emergency department costs or visit rates.
Implications
This real-world analysis of a large, US administrative claims database shows significantly lower medical costs and inpatient resource utilization among patients treated with semaglutide 2.4 mg with overweight or obesity and HF compared with those who did not receive semaglutide 2.4 mg. Improving outcomes with semaglutide 2.4 mg in these patients combined with lower costs and HCRU can help to manage the growing burden of HF to the US.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Clinical therapeutics
医学-药学
CiteScore
6.00
自引率
3.10%
发文量
154
审稿时长
9 weeks
期刊介绍:
Clinical Therapeutics provides peer-reviewed, rapid publication of recent developments in drug and other therapies as well as in diagnostics, pharmacoeconomics, health policy, treatment outcomes, and innovations in drug and biologics research. In addition Clinical Therapeutics features updates on specific topics collated by expert Topic Editors. Clinical Therapeutics is read by a large international audience of scientists and clinicians in a variety of research, academic, and clinical practice settings. Articles are indexed by all major biomedical abstracting databases.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


