婴儿左冠状动脉与肺动脉非缺血性异常的冠状动脉口狭窄。
IF 0.7
Q4 CARDIAC & CARDIOVASCULAR SYSTEMS
Annals of Pediatric Cardiology
Pub Date : 2025-01-01
Epub Date: 2025-07-14
DOI:10.4103/apc.apc_145_25
引用次数: 0
摘要
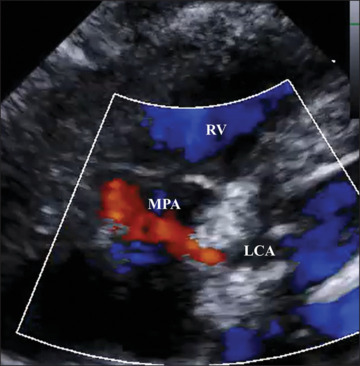
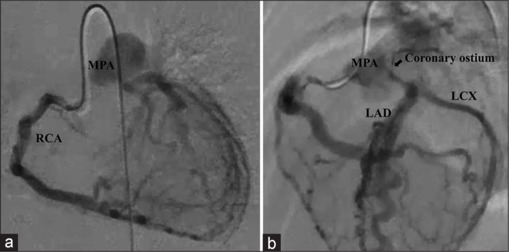
婴儿期诊断的无症状、非缺血性左冠状动脉异常(ALCAPA)的影像学细节尚未得到很好的确定。一个6个月大的女孩被诊断为ALCAPA,但显示正常的左心室收缩。超声心动图及冠状动脉造影显示右冠状动脉至左冠状动脉(LCA)侧支通路丰富,肺动脉开口狭窄至1.5 mm, LCA至肺动脉血流受限。冠状动脉口狭窄可能是无症状、非缺血性ALCAPA的表现之一。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Coronary ostial stenosis in an infant with nonischemic anomalous left coronary artery from the pulmonary artery.
Imaging details of asymptomatic, nonischemic cases of anomalous left coronary artery from the pulmonary artery (ALCAPA) diagnosed in infancy are not well established. A 6-month-old girl was diagnosed with ALCAPA but showed normal left ventricular contraction. Echocardiography and coronary angiography revealed abundant collateral pathways from the right coronary artery to the left coronary artery (LCA), with the opening of the pulmonary artery narrowed to 1.5 mm and a restricted continuous flow from the LCA to the pulmonary artery. Coronary ostial stenosis could be one of the findings in asymptomatic, nonischemic ALCAPA.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Annals of Pediatric Cardiology
CARDIAC & CARDIOVASCULAR SYSTEMS-
CiteScore
1.40
自引率
14.30%
发文量
51
审稿时长
23 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


