预测复发原发性中枢神经系统淋巴瘤的挽救性立体定向放射手术结果:机器学习驱动的决策树分析
IF 5
2区 医学
Q2 Medicine
引用次数: 0
摘要
目的探讨影响复发原发性中枢神经系统淋巴瘤(r-PCNSL)患者行立体定向放射外科挽救治疗(SRS-ST)疗效的关键临床危险因素,并建立基于决策树的预测模型。患者与方法回顾性分析2012年1月至2021年11月在徐州医科大学第二附属医院行SRS-ST的r-PCNSL患者。队列随机分为训练组和验证组(比例为7:3)。采用C5.0算法建立预测治疗反应的决策树模型。使用诊断指标评估模型性能,包括准确性(ACC)、敏感性和特异性。结果入选209例符合纳入/排除标准的患者。生存分析显示,平均无进展生存期(PFS)为7.5±2.6个月,总生存期(OS)为13.8±4.1个月。通过多变量分析,建立了一个包含三个关键预后参数的决策树模型:Karnofsky绩效状态(KPS);脑深部结构受累;以及国际结外淋巴瘤研究组(IELSG)评分。该模型具有较强的预测准确性,训练集的敏感性为0.880-1.000,验证集的敏感性为0.667-0.880,特异性分别为0.926-1.000和0.854-0.984。结论sour分析确定了r-PCNSL患者接受SRS-ST治疗反应的关键决定因素,建立了一种临床适用的决策树模型,指导血液学家和神经肿瘤学家制定个性化的治疗方法。本文章由计算机程序翻译,如有差异,请以英文原文为准。
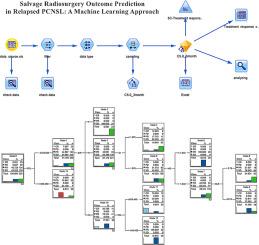
Prognosticating salvage stereotactic radiosurgery outcomes in relapsed primary central nervous system lymphoma: A machine learning-driven decision tree analysis
Purpose
To identify key clinical risk factors affecting therapeutic outcomes in relapsed primary central nervous system lymphoma (r-PCNSL) patients undergoing stereotactic radiosurgery salvage therapy (SRS-ST) and develop a decision tree-based predictive model.
Patients and Methods
A retrospective analysis was performed on r-PCNSL patients undergoing SRS-ST at The Second Affiliated Hospital of Xuzhou Medical University between January 2012 and November 2021. The cohort was randomly divided into training and validation sets (7:3 ratio). The C5.0 algorithm was employed to develop a decision tree model for predicting treatment response. Model performance was evaluated using diagnostic metrics including accuracy (ACC), sensitivity, and specificity.
Results
A cohort of 209 patients meeting inclusion/exclusion criteria were enrolled. Survival analysis revealed a mean progression-free survival (PFS) of 7.5 ± 2.6 months and overall survival (OS) of 13.8 ± 4.1 months. Using multivariate analysis, a decision tree model was developed incorporating three critical prognostic parameters: Karnofsky Performance Status (KPS); deep brain structure involvement; and International Extranodal Lymphoma Study Group (IELSG) score. The model demonstrated robust predictive accuracy, with sensitivities of 0.880-1.000 in the training set versus 0.667-0.880 in the validation set, and corresponding specificities of 0.926-1.000 and 0.854-0.984, respectively.
Conclusions
Our analysis identified critical determinants of therapeutic response in r-PCNSL patients receiving SRS-ST, developing a clinically applicable decision tree model to guide hematologists and neuro-oncologists in personalizing treatment approaches.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Translational Oncology
ONCOLOGY-
CiteScore
8.40
自引率
2.00%
发文量
314
审稿时长
54 days
期刊介绍:
Translational Oncology publishes the results of novel research investigations which bridge the laboratory and clinical settings including risk assessment, cellular and molecular characterization, prevention, detection, diagnosis and treatment of human cancers with the overall goal of improving the clinical care of oncology patients. Translational Oncology will publish laboratory studies of novel therapeutic interventions as well as clinical trials which evaluate new treatment paradigms for cancer. Peer reviewed manuscript types include Original Reports, Reviews and Editorials.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


