过继转移的Th17细胞与宿主B细胞合作,实现持久的肿瘤免疫
IF 44.5
1区 医学
Q1 CELL BIOLOGY
引用次数: 0
摘要
CD4+ T辅助细胞在过继T细胞治疗(ACT)的成功中起着重要作用,但目前尚不清楚哪一种亚群最具治疗性以及它们如何消除肿瘤。我们发现肿瘤特异性Th17细胞比其他CD4+亚群更有效地根除黑色素瘤,并通过独特的宿主免疫协调来防止远处转移。供体Th17细胞需要宿主B细胞(而不是T细胞)才能使肿瘤消退。Th17细胞诱导B细胞增殖、活化和分化,而B细胞通过增强IL-21的产生来增强Th17细胞的多功能性。Th17和B细胞共定位于淋巴组织,Th17细胞通过IL-21的产生和CD40L的共刺激诱导生发中心和肿瘤反应性抗体。此外,这些肿瘤特异性抗体对肿瘤攻击提供部分保护。在此,我们揭示了过继性转移的Th17细胞与B细胞合作驱动持续免疫,证明了内源性B细胞应答在有效CD4+ ACT中的作用。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Adoptively transferred Th17 cells cooperate with host B cells to achieve durable tumor immunity
CD4+ T helper cells play an important role in adoptive T cell therapy (ACT) success, but it remains unclear which subset is most therapeutic and how they eliminate tumors. We find that tumor-specific Th17 cells eradicate melanoma more effectively than other CD4+ subsets and protect against distant metastases by unique orchestration of host immunity. Donor Th17 cells require host B cells —but not T cells— for tumor regression. Th17 cells induce B cell proliferation, activation, and differentiation, while B cells augment Th17 cell polyfunctionality by enhancing IL-21 production. Th17 and B cells colocalize in lymphoid tissues, where Th17 cells induce germinal centers and tumor-reactive antibodies via IL-21 production and CD40L costimulation. Furthermore, these tumor-specific antibodies provide partial protection against tumor challenge. Herein, we reveal that adoptively transferred Th17 cells cooperate with B cells to drive sustained immunity, demonstrating a role for endogenous B cell responses in effective CD4+ ACT.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
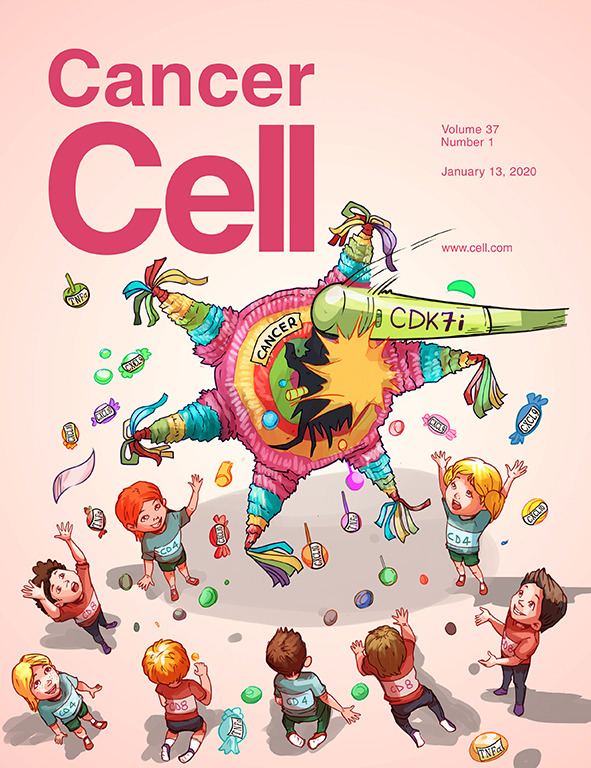
Cancer Cell
医学-肿瘤学
CiteScore
55.20
自引率
1.20%
发文量
179
审稿时长
4-8 weeks
期刊介绍:
Cancer Cell is a journal that focuses on promoting major advances in cancer research and oncology. The primary criteria for considering manuscripts are as follows:
Major advances: Manuscripts should provide significant advancements in answering important questions related to naturally occurring cancers.
Translational research: The journal welcomes translational research, which involves the application of basic scientific findings to human health and clinical practice.
Clinical investigations: Cancer Cell is interested in publishing clinical investigations that contribute to establishing new paradigms in the treatment, diagnosis, or prevention of cancers.
Insights into cancer biology: The journal values clinical investigations that provide important insights into cancer biology beyond what has been revealed by preclinical studies.
Mechanism-based proof-of-principle studies: Cancer Cell encourages the publication of mechanism-based proof-of-principle clinical studies, which demonstrate the feasibility of a specific therapeutic approach or diagnostic test.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


