分析美国常见健康状况的药物遗传学成本效益和节省。
IF 2.9
3区 医学
Q2 GENETICS & HEREDITY
引用次数: 0
摘要
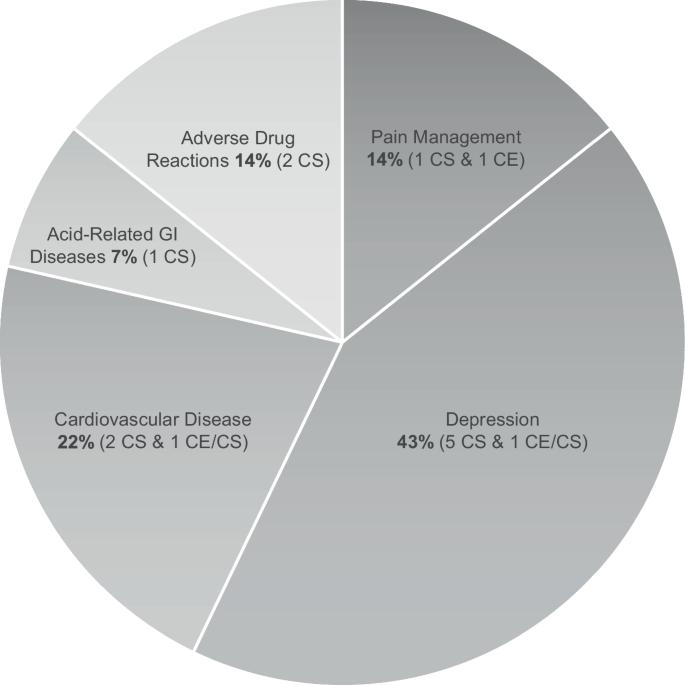
本综述描述了药物遗传学(PGx)的医疗成本效益/节省以及在选定的常见健康状况下的相关临床结果。PGx允许基于基因型和表型的靶向药物治疗。研究强调PGx检测如何通过预测细胞色素P450酶(CYPs)遗传变异和CYP酶表型改变引起的药物相互作用而降低药物不良反应(adr)的发病率和死亡率。尽管有许多可用的PGx检测平台和PGx指导治疗,但由于有限的(1)保险覆盖范围和检测报销以及药剂师解释,(2)结果数据,如证据显示预防性PGx检测对疗效或预防不良反应的益处,以及(3)PGx检测在医疗保健专业人员中的推广,临床实施仍然具有挑战性和缓慢。其中,成本是患者和医疗保健系统面临的最大障碍。这篇综述描述了PGx检测如何对支付者和医疗保健系统具有成本效益或节省成本,特别是对抑郁症、心血管疾病和不良反应。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Analyzing pharmacogenetics cost effectiveness and savings across common health conditions in the United States
This review describes healthcare cost effectiveness/savings for pharmacogenetics (PGx) and relevant clinical outcomes in selected common health conditions. PGx allows targeted drug treatment based on genotype and phenotype. Studies highlight how PGx testing reduces the morbidity and mortality of adverse drug reactions (ADRs) by predicting unexpected drug metabolism due to genetic variation in cytochrome P450 enzymes (CYPs) and drug-drug interactions caused by altered CYP enzyme phenotype. Despite many available PGx testing platforms and PGx-guided treatments, clinical implementation remains challenging and slow due to limited (1) insurance coverage and reimbursement of testing and pharmacist interpretation, (2) outcome data such as evidence showing the benefits of preemptive PGx testing for efficacy or ADR prevention, and (3) promotion of PGx testing among healthcare professionals. Of these, cost is the most significant barrier to patients and the healthcare system. This review describes how PGx testing can be cost effective or cost saving for payors and the healthcare system, especially for depression, cardiovascular disease, and ADRs.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Pharmacogenomics Journal
医学-药学
CiteScore
7.20
自引率
0.00%
发文量
35
审稿时长
6-12 weeks
期刊介绍:
The Pharmacogenomics Journal is a print and electronic journal, which is dedicated to the rapid publication of original research on pharmacogenomics and its clinical applications.
Key areas of coverage include:
Personalized medicine
Effects of genetic variability on drug toxicity and efficacy
Identification and functional characterization of polymorphisms relevant to drug action
Pharmacodynamic and pharmacokinetic variations and drug efficacy
Integration of new developments in the genome project and proteomics into clinical medicine, pharmacology, and therapeutics
Clinical applications of genomic science
Identification of novel genomic targets for drug development
Potential benefits of pharmacogenomics.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


