在癌症实验模型中通过定制化学诱变诱导错配修复缺陷基因型
IF 44.5
1区 医学
Q1 CELL BIOLOGY
引用次数: 0
摘要
错配修复缺陷(MMRd)肿瘤含有数千个富含插入-删除(indels)的体细胞突变,赋予免疫治疗高敏感性。我们试图使用诱变剂在免疫抗性细胞中设计MMRd基因型来复制这种表型。替莫唑胺(TMZ)和顺铂联合使用可导致小鼠细胞系中因Msh2的表观遗传缺失而富集的高突变负荷的快速积累。预处理细胞对PD-1阻断反应敏感。在不影响健康组织的情况下,用TMZ、顺铂和抗pd -1免疫耐药肿瘤细胞进行全身治疗,可提高生存率、瘤内T细胞浸润和下调Msh2表达。在18例难治性错配修复熟练的结直肠癌患者的临床试验中,没有看到反应,但在无细胞DNA中出现了MMRd特征。这些发现表明,通过化学诱变重述MMRd基因型可以产生免疫原性表型。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Induction of a mismatch repair deficient genotype by tailored chemical mutagenesis in experimental models of cancer
Mismatch repair deficient (MMRd) tumors harbor thousands of somatic mutations enriched for insertion–deletion (indels) conferring high sensitivity to immunotherapy. We sought to reproduce this phenotype using mutagenic agents to engineer an MMRd genotype in immunoresistant cells. The combination of temozolomide (TMZ) and cisplatin led to a rapid accumulation of a high mutational load enriched for indels in murine cell lines resulting from the epigenetic loss of Msh2. Pretreated cells showed sensitivity to PD-1 blockade. Systemic treatment with TMZ, cisplatin, and anti-PD-1 bearing immunoresistant tumor cells led to increased survival, intratumoral T cell infiltration, and downregulation of Msh2 expression without affecting healthy tissues. In a clinical trial with 18 patients with refractory mismatch repair proficient colorectal cancer, no responses were seen, but MMRd signatures emerged in cell-free DNA. These findings show that recapitulating an MMRd genotype through chemical mutagenesis can generate an immunogenic phenotype.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
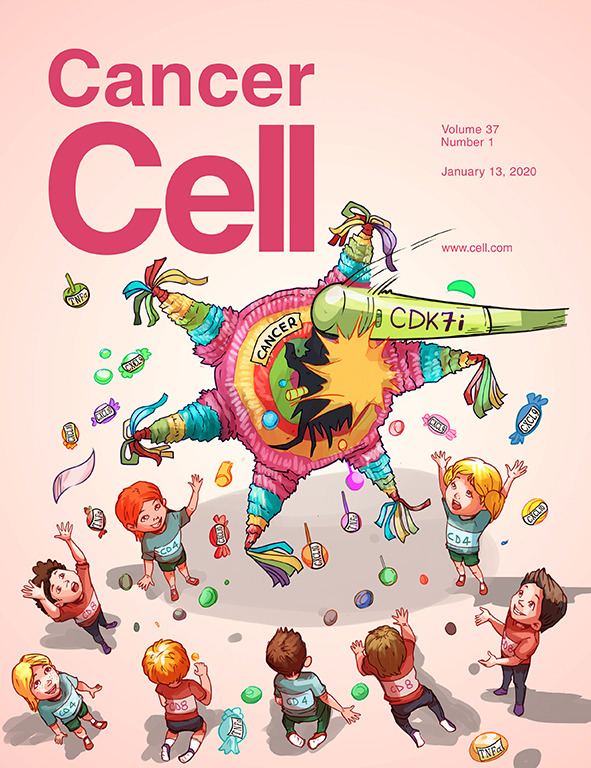
Cancer Cell
医学-肿瘤学
CiteScore
55.20
自引率
1.20%
发文量
179
审稿时长
4-8 weeks
期刊介绍:
Cancer Cell is a journal that focuses on promoting major advances in cancer research and oncology. The primary criteria for considering manuscripts are as follows:
Major advances: Manuscripts should provide significant advancements in answering important questions related to naturally occurring cancers.
Translational research: The journal welcomes translational research, which involves the application of basic scientific findings to human health and clinical practice.
Clinical investigations: Cancer Cell is interested in publishing clinical investigations that contribute to establishing new paradigms in the treatment, diagnosis, or prevention of cancers.
Insights into cancer biology: The journal values clinical investigations that provide important insights into cancer biology beyond what has been revealed by preclinical studies.
Mechanism-based proof-of-principle studies: Cancer Cell encourages the publication of mechanism-based proof-of-principle clinical studies, which demonstrate the feasibility of a specific therapeutic approach or diagnostic test.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


