CSF1R+骨髓单核细胞驱动CAR-T细胞抵抗侵袭性B细胞淋巴瘤
IF 44.5
1区 医学
Q1 CELL BIOLOGY
引用次数: 0
摘要
尽管有改善,但大约60%的复发或难治性(r/r)侵袭性B细胞淋巴瘤(B- nhl)患者不能从CAR-T细胞治疗中获得持久的益处。为了阐明与CAR-T治疗耐药相关的因素,我们对CAR-T前和CAR-T后细胞标本进行了高维分析。在非持久反应的患者中,我们发现了与预后相关的淋巴瘤相关骨髓单核细胞(LAMM)基因特征。深入分析显示,在人和小鼠B-NHL中,不同的CSF1R+CD14+CD68+ LAMM细胞群抑制CAR-T细胞功能,并与不良预后相关。细胞-细胞推理分析发现,LAMM细胞通过PGE2-EP2/EP4轴直接与LAMM- t细胞相互作用,从而损害CAR-T细胞的功能。在原发性淋巴瘤小鼠模型中,联合抗cd19 CAR-T细胞治疗与CSF1R阻断表现出协同作用并提高生存率。这些发现为联合使用抗cd19 CAR-T细胞和CSF1R抑制剂治疗r/r侵袭性B-NHL患者提供了强有力的理论依据。本文章由计算机程序翻译,如有差异,请以英文原文为准。

CSF1R+ myeloid-monocytic cells drive CAR-T cell resistance in aggressive B cell lymphoma
Despite the improvement, approximately 60% of patients with relapsed or refractory (r/r) aggressive B cell lymphoma (B-NHL) do not achieve durable benefit from CAR-T cell therapy. To elucidate factors associated with CAR-T therapy resistance, we conducted high-dimensional analyses of pre- and post-CAR-T cell specimens. In patients with non-durable response, we identified a prognostically relevant lymphoma-associated myeloid-monocytic (LAMM) gene signature. In-depth profiling revealed a distinct CSF1R+CD14+CD68+ LAMM cell population in both human and murine B-NHL that inhibits CAR-T cell function and correlates with poor outcome. Cell-cell inference analysis uncovered that LAMM cells impair CAR-T cell function through a direct LAMM-T cell interaction via the PGE2-EP2/EP4 axis. In an autochthonous lymphoma mouse model, combined anti-CD19 CAR-T cell therapy with CSF1R blockade exhibited synergistic effects and improved survival. These findings provide strong rationale for combining anti-CD19 CAR-T cells with CSF1R inhibitors in treating r/r aggressive B-NHL patients.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
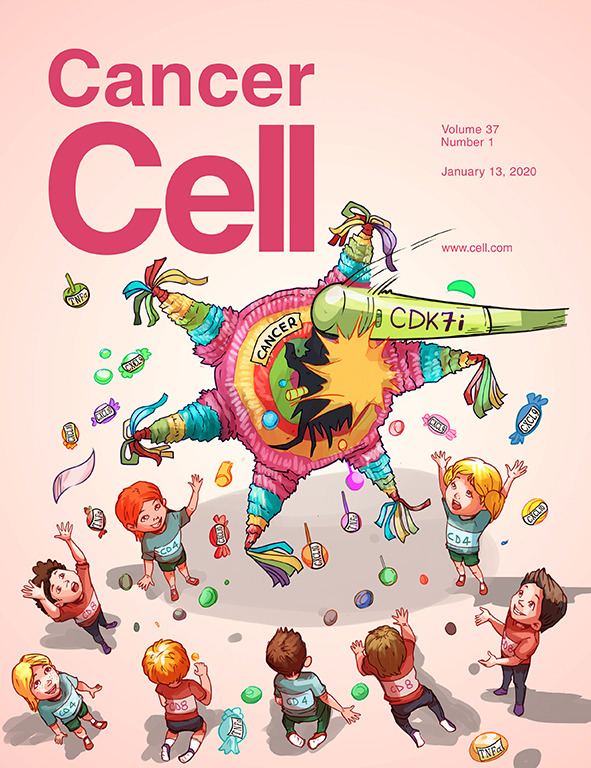
Cancer Cell
医学-肿瘤学
CiteScore
55.20
自引率
1.20%
发文量
179
审稿时长
4-8 weeks
期刊介绍:
Cancer Cell is a journal that focuses on promoting major advances in cancer research and oncology. The primary criteria for considering manuscripts are as follows:
Major advances: Manuscripts should provide significant advancements in answering important questions related to naturally occurring cancers.
Translational research: The journal welcomes translational research, which involves the application of basic scientific findings to human health and clinical practice.
Clinical investigations: Cancer Cell is interested in publishing clinical investigations that contribute to establishing new paradigms in the treatment, diagnosis, or prevention of cancers.
Insights into cancer biology: The journal values clinical investigations that provide important insights into cancer biology beyond what has been revealed by preclinical studies.
Mechanism-based proof-of-principle studies: Cancer Cell encourages the publication of mechanism-based proof-of-principle clinical studies, which demonstrate the feasibility of a specific therapeutic approach or diagnostic test.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


