国内专家对前交叉韧带重建失败与修复的共识
IF 5.9
1区 医学
Q1 ORTHOPEDICS
引用次数: 0
摘要
背景:近年来,随着中国前交叉韧带(ACL)重建手术的增加,手术失败率也相应增加。原发性手术技术的多变性和手术失败机制的复杂性给手术失败的诊断、手术计划和手术修复带来了巨大的挑战。方法为了应对这些挑战,中国骨科医师协会(CAOS)和中国运动医学学会(CSSM)发起了关于ACL重建失败和修复的专家共识。采用改进的德尔菲法,邀请国内相关领域的67位专家进行共识制定和评审。结果专家小组在12个关键方面达成了高度共识。共识清楚地定义了ACL重建失败,并概述了多种因素,其中手术错误,特别是不正确的骨隧道放置,被认为是主要原因。它还强调了患者特定变量对失败可能性的重大影响。翻修手术的建议包括仔细确定翻修指征,保留半月板完整性以降低关节退变的风险,以及根据患者的个人评估选择单期或两期手术。目前还没有统一的骨缺损治疗方法,需要进行全面的评估。移植物的选择应针对每位患者,自体移植物、同种异体移植物或合成韧带都是可行的选择。对于枢轴移位试验呈高阳性或从事高要求运动的患者,建议前外侧结构增强或重建。结论共识强调了ACL翻修手术中个性化入路的重要性。通过明确定义失败标准和概述手术修正策略,这些声明有望作为改进临床实践,减少并发症和改善手术结果的指南。1)循证临床指南的建立:本文提出了严格发展的ACL重建失败和修复的专家共识,提供了直接适用于手术实践的循证临床指南。跨医疗机构的这些协议的标准化有可能减少患者护理的可变性,并在全国范围内改善手术结果。2)ACL手术精准医学的进步:通过强调在ACL重建失败的管理中需要针对患者的方法,这一共识支持了骨科手术精准医学的进步。对移植物选择、手术技术和康复方案的量身定制的建议可以带来更个性化和有效的治疗,降低并发症的风险,提高康复。3)手术技术创新的催化剂:本文指出了当前ACL翻修实践中的关键差距和挑战,为未来的研究和创新提供了基础。通过概述手术决策的复杂性和争议,这项工作可以促进新的手术技术和技术的发展,旨在改善患者的预后。4)未来研究和发展框架:该共识不仅解决了当前的临床需求,而且为ACL翻修的未来研究设定了明确的议程。通过提供一种结构化的方法来诊断和管理ACL失败,本文指导了基础和转化研究工作,确保未来的创新与临床现实和患者需求保持一致。本文章由计算机程序翻译,如有差异,请以英文原文为准。
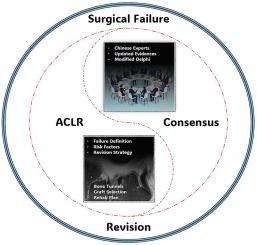
Chinese expert consensus on failure and revision after anterior cruciate ligament reconstruction
Background
With the recent rise in anterior cruciate ligament (ACL) reconstruction surgeries in China, a corresponding increase in surgical failures has been observed. Variability in primary surgical techniques and the intricacies of failure mechanisms have introduced significant challenges in diagnosing failures, planning procedures, and conducting revision surgeries.
Methods
In response to these challenges, the Chinese Association of Orthopaedic Surgeons (CAOS) and the Chinese Society of Sports Medicine (CSSM) initiated the development of an expert consensus on ACL reconstruction failure and revision. Utilizing a modified Delphi method, 67 domestic experts from relevant fields were invited for consensus formulation and review.
Results
The expert panel achieved a high degree of consensus on twelve key aspects. The consensus clearly defines ACL reconstruction failure and outlines multiple contributing factors, with surgical errors, especially incorrect bone tunnel placement, identified as primary causes. It also emphasizes the significant impact of patient-specific variables on the likelihood of failure. Recommendations for revision surgeries include careful determination of revision indications, preserving meniscal integrity to reduce the risk of joint degeneration, and a preference for single-stage or two-stage surgeries based on individual patient evaluations. A unified approach for managing bone defects remains absent, necessitating comprehensive assessments. Graft selection should be tailored to each patient, with autografts, allografts, or synthetic ligaments as viable options. For patients with a highly positive pivot shift test or those engaged in high-demand athletic activities, anterolateral structure augmentation or reconstruction is recommended.
Conclusion
The consensus emphasizes the critical need for individualized approaches in ACL revision surgery. By clearly defining failure criteria and outlining strategies for surgical revisions, these statements are expected to serve as a guide for refining clinical practice, reducing complications, and improving surgical outcomes.
The translational potential of this article
- 1)Establishment of Evidence-Based Clinical Guidelines: This article presents a rigorously developed expert consensus on ACL reconstruction failure and revision, providing evidence-based clinical guidelines that are directly applicable in surgical practice. The standardization of these protocols across medical institutions has the potential to reduce variability in patient care and improve surgical outcomes on a national scale.
- 2)Advancement of Precision Medicine in ACL Surgery: By emphasizing the need for patient-specific approaches in the management of ACL reconstruction failure, this consensus supports the advancement of precision medicine in orthopaedic surgery. The tailored recommendations for graft selection, surgical techniques, and rehabilitation protocols can lead to more personalized and effective treatments, reducing the risk of complications and enhancing recovery.
- 3)Catalyst for Innovation in Surgical Techniques: The article identifies critical gaps and challenges in current ACL revision practices, providing a foundation for future research and innovation. By outlining the complexities and controversies in surgical decision-making, this work serves as a catalyst for the development of new surgical techniques and technologies aimed at improving patient outcomes.
- 4)Framework for Future Research and Development: The consensus not only addresses immediate clinical needs but also sets a clear agenda for future research in ACL revision. By offering a structured approach to the diagnosis and management of ACL failures, this article guides both basic and translational research efforts, ensuring that future innovations are aligned with clinical realities and patient needs.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Journal of Orthopaedic Translation
Medicine-Orthopedics and Sports Medicine
CiteScore
11.80
自引率
13.60%
发文量
91
审稿时长
29 days
期刊介绍:
The Journal of Orthopaedic Translation (JOT) is the official peer-reviewed, open access journal of the Chinese Speaking Orthopaedic Society (CSOS) and the International Chinese Musculoskeletal Research Society (ICMRS). It is published quarterly, in January, April, July and October, by Elsevier.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


