炎症与精神分裂症患者皮质纹状体奖赏回路的进化和静息状态功能连接减少有关。
IF 6.6
1区 医学
Q1 NEUROSCIENCES
引用次数: 0
摘要
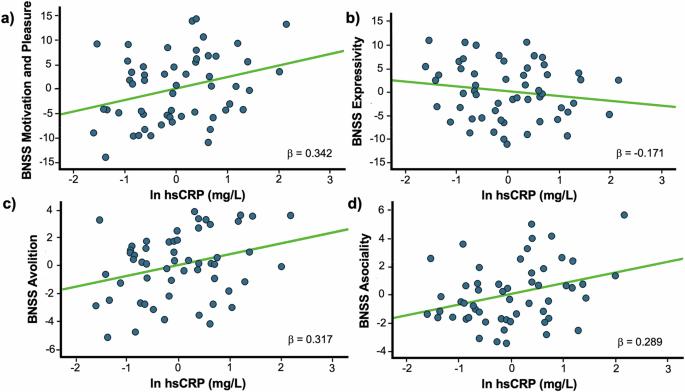
轻度炎症与精神分裂症患者的阴性症状有关。在这些症状中,动机和快乐方面的缺陷,尤其是在自由领域的缺陷,尤其令人致残。炎症对抑郁症患者动机缺陷的影响与涉及下腹侧纹状体(iVS)和腹内侧前额叶皮层(vmPFC)的皮质纹状体奖励回路的破坏有关。因此,我们研究了精神分裂症患者的炎症、阴性症状和皮质纹状体奖赏回路之间的关系。57例精神分裂症患者均出现阴性症状和高敏感性c反应蛋白(hsCRP)。从这些个体的43个子集中获得静息状态功能连接(rsFC)。测试了hsCRP与短暂阴性症状量表(BNSS)的动机与愉悦(MAP)和表达性(EXP)维度以及iVS和vmPFC之间的靶向rsFC之间的关联。所有统计模型中的协变量包括年龄、性别、种族、吸烟、体重指数、抑郁症和氯丙嗪当量。hsCRP与BNSS MAP显著相关(β = 0.34, pcorr = 0.022),特别是在自发性和社会性领域(p corr = 0.57)或钝化情感和痛症领域(p均为0.05)。hsCRP还与右iVS到vmPFC的rsFC降低显著相关(β=-0.37, pcorr = 0.029),这反过来又与较高(hsCRP >2 mg/L)但不降低炎症的个体的血糖升高相关(β=-14.01, p = 0.007 vs. β= 0.07, p = 0.77)。hsCRP与精神分裂症患者的自发性和皮质纹状体rsFC减少以及炎症增加有关,强调需要进一步研究来复制这些与精神分裂症患者亚组大脑连通性变化的关联。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Inflammation is associated with avolition and reduced resting state functional connectivity in corticostriatal reward circuitry in patients with schizophrenia
Low-grade inflammation has been associated with negative symptoms in patients with schizophrenia. Of these symptoms, deficits in motivation and pleasure, especially in the domain of avolition, are particularly disabling. Effects of inflammation on motivational deficits in patients with depression are associated with disruptions in corticostriatal reward circuitry involving the inferior ventral striatum (iVS) and ventromedial prefrontal cortex (vmPFC). Accordingly, we examined the relationships among inflammation, negative symptoms, and corticostriatal reward circuitry in patients with schizophrenia. Negative symptoms and high sensitivity C-reactive protein (hsCRP) were obtained in 57 individuals with schizophrenia. Resting state functional connectivity (rsFC) was obtained from a subset of 43 of these individuals. Associations were tested between hsCRP and the motivation and pleasure (MAP) and expressivity (EXP) dimensions of the Brief Negative Symptom Scale (BNSS) as well as targeted rsFC between iVS and vmPFC. Covariates in all statistical models included age, sex, race, smoking, body mass index, depression, and chlorpromazine equivalents. hsCRP was significantly associated with BNSS MAP (β = 0.34, pcorr = 0.022, specifically the domains of avolition and asociality (p < 0.05), but not BNSS EXP (β = −0.17, pcorr = 0.57) or the domains of blunted affect or alogia (both p > 0.05). hsCRP was also significantly associated with decreased rsFC from right iVS to vmPFC (β=−0.37, pcorr = 0.029), which in turn, was associated with increased avolition in individuals with higher (hsCRP >2 mg/L) but not lower inflammation (β=−14.01, p = 0.007 vs. β = 0.07, p = 0.77, respectively). hsCRP was associated with reduced avolition and corticostriatal rsFC in patients with schizophrenia and increased inflammation, underscoring the need for further research to replicate these associations with brain connectivity changes in this subgroup of individuals with schizophrenia.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Neuropsychopharmacology
医学-精神病学
CiteScore
15.00
自引率
2.60%
发文量
240
审稿时长
2 months
期刊介绍:
Neuropsychopharmacology is a reputable international scientific journal that serves as the official publication of the American College of Neuropsychopharmacology (ACNP). The journal's primary focus is on research that enhances our knowledge of the brain and behavior, with a particular emphasis on the molecular, cellular, physiological, and psychological aspects of substances that affect the central nervous system (CNS). It also aims to identify new molecular targets for the development of future drugs.
The journal prioritizes original research reports, but it also welcomes mini-reviews and perspectives, which are often solicited by the editorial office. These types of articles provide valuable insights and syntheses of current research trends and future directions in the field of neuroscience and pharmacology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


