低肌肉质量对肺移植患者临床预后的影响。
IF 4.4
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
Journal of Thoracic and Cardiovascular Surgery
Pub Date : 2025-10-01
DOI:10.1016/j.jtcvs.2025.03.030
引用次数: 0
摘要
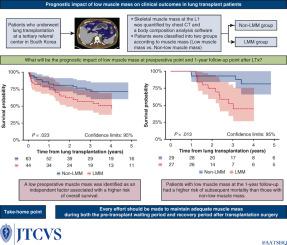
背景:低肌肉量(LMM)被认为是各种慢性肺部疾病的不良预后因素。然而,其对肺移植受者的预后影响仍不确定。方法:我们回顾性分析了在韩国三级转诊中心接受肺移植的患者。使用市售的身体成分分析软件,通过胸部计算机断层扫描在L1椎体水平量化移植前骨骼肌质量。使用先前在韩国人群中验证的LMM阈值将患者分为LMM和非LMM组。然后我们评估术前LMM对肺移植后临床结果的预后影响。结果:本组共纳入107例患者,其中LMM组44例(41.1%)。移植后中位随访时间为958天。术前LMM被确定为与总死亡率较高风险相关的独立因素(调整后HR 2.15, 95% CI 1.07-4.34)。此外,LMM患者发生原发性移植物功能障碍的风险更高(调整后OR为3.56,95% CI为1.25-10.18)。在1年的随访中,37.5%的基线LMM患者恢复,并被重新分类为非LMM组,这种改善被发现减轻了术前LMM的负面影响。结论:移植前LMM与肺移植受者不良临床预后显著相关。这些发现强调了在肺移植等待期保持足够的肌肉质量的重要性。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Prognostic impact of low muscle mass on clinical outcomes in patients who undergo lung transplant
Background
Low muscle mass (LMM) is recognized as a poor prognostic factor in various chronic lung diseases. However, its prognostic impact on recipients of lung transplants remains inconclusive.
Methods
We retrospectively analyzed patients who underwent lung transplantation at a tertiary referral center in South Korea. Pretransplant skeletal muscle mass was quantified at the L1 vertebral level by computed tomography scans of the chest using a commercially available body composition analysis software. Patients were classified into LMM and non-LMM group using a threshold for LMM that had been previously validated in the South Korean population. We then evaluated the prognostic impact of preoperative LMM on clinical outcomes after lung transplantation.
Results
A total of 107 patients were included in this analysis, of whom 44 (41.1%) were classified into the LMM group. The median follow-up duration was 958 days posttransplantation. A preoperative LMM was identified as an independent factor associated with a greater risk of overall mortality (adjusted hazard ratio, 2.15; 95% confidence interval, 1.07-4.34). In addition, patients with LMM had a greater risk of developing primary graft dysfunction (adjusted odds ratio, 3.56; 95% confidence interval, 1.25-10.18). At the 1-year follow-up, 37.5% of the patients with baseline LMM had recovered and were reclassified into the non-LMM group, and this improvement was found to mitigate the negative impact of preoperative LMM.
Conclusions
Pretransplant LMM was significantly associated with poor clinical outcomes in recipients of lung transplants. These findings highlight the importance of maintaining adequate muscle mass during the waiting period for lung transplantation.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
11.20
自引率
10.00%
发文量
1079
审稿时长
68 days
期刊介绍:
The Journal of Thoracic and Cardiovascular Surgery presents original, peer-reviewed articles on diseases of the heart, great vessels, lungs and thorax with emphasis on surgical interventions. An official publication of The American Association for Thoracic Surgery and The Western Thoracic Surgical Association, the Journal focuses on techniques and developments in acquired cardiac surgery, congenital cardiac repair, thoracic procedures, heart and lung transplantation, mechanical circulatory support and other procedures.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


